Get Complete Project Material File(s) Now! »
Chapter 3: Characterisation of the light-damaged albino rat as an animal model of age-related macular degeneration
Introduction
Age-related macular degeneration (AMD) is the major cause of blindness in people aged 75 years or older in developed countries and the third cause of blindness in the world, following cataract and glaucoma (Klaver et al., 1998b; Biarnés et al., 2011). Pathologically, AMD is characterised by accumulation of deposits between the retinal pigment epithelium (RPE) and the choroid, called drusen. During early AMD, drusen can be hard with distinct margins, which is characteristic of the dry form of AMD. Subsequently, choroidal neovascularisation develops and is accompanied by increased vascular leakage, which represents the wet form of AMD (de Jong, 2006). So far, there is no strategy that can cure AMD or an established effective treatment for early stage of AMD. The current management for the disease is mainly focused on the pathological progression in the late stage. The aim of this study is to analyse how the damaging process is initiated and progresses at the early stage of AMD by using a light-damaged albino rat model.
The albino rat exposed to intense fluorescent light has been an animal model of retina degeneration since the 1960s (Noell et al., 1966). Histological analysis of the light-damaged animal model has shown changes to Müller cells, loss of photoreceptors and pigment epithelium, breakage to Bruch’s membrane, and choroidal damage. These are all very similar characteristics to those observed in human AMD (Noell et al., 1966; van Best et al., 1997; Wu et al., 2005; Marc et al., 2008). In the light-damaged albino rat eye, the injured area is regional and mainly limited to the central and superior segments of the retina (Marc et al., 2008). In addition to the histological changes, neural dysfunction has been found in this animal model, particularly seen as a reduction in the a- and b-waves in a full-field retinal electroretinogram (ERG) (Noell et al., 1966; Penn et al., 1989). The mechanisms of retinal degeneration in the animal model induced by light-damage, however, still remains unclear. We hypothesise that in the light-damaged animal model there is a complex procedure involving oxidative stress, inflammation and vascular reactions that mimics the disease process. The retinal stress initiated by excessive rhodopsin bleaching will consequently spread damage into the RPE and choriocapillaris.
Oxidative stress in photoreceptors results from the process of photo-oxidation generated by rhodopsin bleaching in photoreceptor outer segments and is also observed in the RPE as a result of phagocytosis of the outer segment (Beatty et al., 2000; Khandhadia & Lotery, 2010). In addition to photoreceptor outer segments, oxidative stress has also been found in the mitochondrial DNA (mtDNA) in photoreceptors from aged human donor tissues (Barron et al., 2001). In the light-damaged animal model, protein nitration has been found to be increased in the photoreceptor outer segment and the RPE when compared to the animals maintained in the dark (Miyagi et al., 2002; Palamalai et al., 2006).
Inflammation is involved in the pathogenesis of AMD (Anderson et al., 2002a; Gupta et al., 2003; Wu et al., 2003; Coorey et al., 2012; Khandhadia et al., 2012), and has also been found in the light-damaged animal model (Zhang et al., 2005; Ng et al., 2009; Rutar et al., 2010; Rutar et al., 2011a; Rutar et al., 2012a). Although the adult retina is regarded as an immune-privileged tissue, it has residential glial cells to provide support and protection of the retinal neurons by supplying nutrients, removing neural waste products and phagocytosis of neuronal debris (Coorey et al., 2012). Retinal microglia become activated after light damage and migrate to the outer retina in a number of animal models (Ng & Streilein, 2001; Zhang et al., 2005; Ni et al., 2008; Xu et al., 2008a; Rutar et al., 2010). Studies of human post-mortem tissue from AMD diagnosed donors have revealed comparable findings with microglial migration to the outer nuclear layer and subretinal space (Gupta et al., 2003; Milam et al., 2003). The inflammatory response is present in both the retina and the choroid following light damage (Rutar et al., 2010), suggesting residential microglia/macrophage activation and migration may play an important role in the process of tissue damage in the light-damaged albino animal model.
Intercellular gap junction channels allow rapid exchange of ions, messengers and metabolic molecules between neighbouring cells. The role of intercellular communication affects a wide range of cellular activities, including signalling, differentiation and growth (Goodenough et al., 1996). In the retina, gap junctions participate in electrical coupling between cells for light sensation (Veruki & Hartveit, 2002; Goodenough & Paul, 2003). Within the rat retina, Cx37 and Cx40 are expressed in the endothelium of large radiating arterioles (Kuo et al., 2008). In rat and mouse retina, both Cx36 and Cx45 are expressed on 88
AII amacrine cells (Söhl et al., 1998; Maxeiner et al., 2005; Veruki & Hartveit, 2009), which are the key elements of the light signal transduction pathways. Hence, both connexin proteins may contribute to coupling function changes in response to light. For example, light modulates the density of gap junctions located on the horizontal cells. By using quantitative freeze-fracture replica methods, enhancement in the density of gap junctions on horizontal cells in gold fish has been found to be associated with dark adaptation (Kurz-Isler & Wolburg, 1986). The light-adapted retina shows an overall increase in alpha ganglion cell coupling at coupled cell number and coupled field compared with the dark-adapted retina (Hu et al., 2010). However, there are very few reports of changes in connexin proteins in the light-damaged animal model.
Cx43 is the most ubiquitous gap junction protein and is expressed by astrocytes and endothelium in the nervous system. Previous studies have demonstrated that it is expressed on Müller cells, astrocytes, vascular endothelium and retinal pigment epithelium in both human and rat retinas (Zahs et al., 2003; Kuo et al., 2008; Kerr et al., 2010). Cx43 plays an important role in modulating response to injury (Danesh-Meyer et al., 2008; O’Carroll et al., 2008; Kerr et al., 2011; Ly et al., 2011; Danesh-Meyer et al., 2012; Davidson et al., 2012a). Increased Cx43 protein and/or transcript have been found in many human CNS injuries and diseases, including stroke, epilepsy and Huntington’s disease (Elisevich et al., 1997; Vis et al., 1998; Nakase et al., 2006).
Based on previous studies, we hypothesise that the injury process in the light-damaged animal model is happening through a complex procedure involving oxidative stress, inflammation and vascular reaction. The retinal stress may be initiated by excessive bleaching of rhodopsin in the photoreceptors from prolonged exposure to the intense light, which would consequently impact on the RPE and choroidal capillaries (Noell et al., 1966; Williams & Howell, 1983). A disruption of the outer retinal blood barrier, mainly the RPE, which involves processes of abnormal cation influx, oxidative damage, and activation of inflammatory response, would lead to secondary injury of the retinal neurons and result in retinal degeneration (Ablonczy et al., 2000; Vaughan et al., 2003; Zhang et al., 2005; Rutar et al., 2010; Rutar et al., 2011a; Rutar et al., 2011b; Rutar et al., 2012a). Oxidative damage and its associated inflammatory response are sufficient to produce retinal lesions in the retina 89 and the choroid (Hollyfield et al., 2008). Alterations in gap junctions expressed on retinal neurons together with photoreceptor degeneration may contribute to the photoreceptor and post-photoreceptor dysfunction in the retina in the animal model. Similar to other animal injury models, Cx43 expression may be affected following intense light-induced injury.
The features of the animal model and its usefulness for its understanding the mechanisms that contribute to AMD are investigated in this chapter. The aim of this study was to evaluate changes in neuronal function, oxidative stress, inflammatory response and the expression of connexin proteins, especially Cx43, in the light-damaged rat retina. In particular, ERG was used to characterise the function of rod and cone pathways; immunohistochemistry and Western blot were employed to correlate the retinal function with cell death, changes in gap junction proteins, oxidative stress, inflammatory responses and RPE alterations.
Materials and methods
Animal handling and light exposure protocol
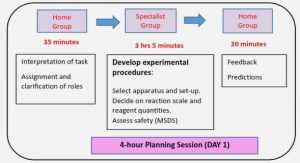
The experimental protocol consists of exposing animals to intense light followed by variable periods of recovery. Briefly, the 24 hours intense light exposure protocol was employed (Yu et al., 2007). Non-exposed animals were used in the control group. The rats were culled after ERG testing either immediately (0 hour), at 6, 24, 48 hours or 7 days after light-exposure. The number of animals used to characterise this light-damaged model is listed in Table 3-1. Animal groups in this study are described in Figure 3-1.
ERG recording
The animals were dark-adapted overnight for 12-14 hours before the ERG recording using a procedure adapted from a previous study (Vessey et al., 2011). Briefly, the animals were anesthetised and ERGs were recorded on the left eye. The light stimulus was elicited by twin-flashes (0.8 ms second stimulus interval) via a Ganzfeld sphere. Flash intensity range was from -2.9 to 2.1 log cd.s/m2. Waveforms were recorded and amplitudes of a- and b-waves from the mixed rod and cone responses were analysed using the Michaelis-Menten function. The implicit times of a- and b-waves were measured from the stimulus onset to the trough of the a-wave or the peak of the b-wave respectively (Sun et al., 2007; Vessey et al., 2011). Oscillatory potentials (OPs) were collected at 2.1 log cd.s/m2.
Chapter 1: Regulation of intercellular communication – seeking a novel therapeutic target for age-related macular degeneration
1.1 Anatomy and physiology of the retina
1.2 Gap junctional communication in physiological and pathological conditions
1.3 Connexin43
1.4 Age-related macular degeneration
1.5 Intense light-exposed albino rat as an animal model for AMD
1.6 Objectives of this study
Chapter 2: Material and methods
2.1 Animals and light damage procedure
2.2 Electroretinogram (ERG) procedure and data analysis
2.3 Immunohistochemistry
2.4 Specific staining
2.5 Imaging
2.6 Collection of human normal and AMD ocular specimens
2.7 Western blot
2.8 Statistical analysis
Chapter 3: Characterisation of the light-damaged albino rat as an animal model of agerelated macular degeneration
3.1 Introduction
3.2 Materials and methods
3.3 Results
3.4 Discussion
Chapter 4: Connexin43 mimetic peptide improves retinal function in the light-damaged animal model of age-related macular degeneration
4.1 Introduction
4.2 Methods
4.3 Results
4.4 Discussion
Chapter 5: Characterisation of gap junction protein connexin43 expression, oxidative stress and inflammation in human age-related macular degeneration
5.1 Introduction
5.2 Materials and methods
5.3 Results
5.4 Discussion
Chapter 6: General discussion and conclusions
6.1 Summary of findings
6.2 A grand synthesis of peptide5 functioning mechanism
6.3 Clinical highlights, limitations of the current study and future directions
6.4 Conclusions
GET THE COMPLETE PROJECT