Get Complete Project Material File(s) Now! »
DEFINITIONS OF QUALITY
To date, there is no universally accepted definition of “quality” within the global health care community. Generally, the following definition from the United States Institute of Medicine (IOM) is used: “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (FMOH 2016:12).
In Ethiopia, as highlighted in the HSTP, quality and equity are defined together, believing that the two must go hand-in-hand. Through various consultative processes, the domains that have been prioritized in this strategy are safe, effective, patient-centered, efficient, accessible, comprehensive, accessible, comprehensive, affordable, and timely. With these prioritised domains, quality in Ethiopia is defined as “comprehensive care that is measurably safe, effective, patient-centered, and uniformly delivered in a timely way that is affordable to the Ethiopian population and appropriately utilises resources and service efficiently” (FMOH 2016:13).
A concise, meaningful and generally applicable definition of quality in all fields and professions including health care is difficult to arrive at. Quality may be looked at from two perspectives, either by the service provider, which is furnishing service, or by the consumer, who is supposed to have received quality service. There is growing consensus that what the service provider believes in as quality service may not hold true for the consumer (Delisa, Gans, Walsh & Bocked 2004:530).
Health providers, therefore, need to measure the quality of their services to meet the needs and expectations of consumers. This contributes to improvement through a specific sort of practice, intervention, or policy that aims at the targeted population.
Dimensions of quality
Six Domains of health care quality as defined by the Institute of Medicine (IOM) are:
• Safe: avoiding injuries to patients from the care that is intended to help them; the WHO defines “patient safety” as the prevention of errors and adverse effects to patients associated with health care.
• Effective: providing services based on scientific knowledge to all who could benefit, and refraining from providing services to those not likely to benefit.
• Patient-centered: providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions.
• Timely: reducing waits and sometimes-harmful delays for both those who receive and those who give care.
• Efficient: avoiding waste, including waste of equipment, supplies, ideas, and energy.
• Equitable: providing care that does not vary in quality because of personal characters tics such as gender, ethnicity, geographic location, and socioeconomic status (Beattie 2012:288-304).
Healthcare facilities receive demands from accreditation organizations, community driven committees, and external customers in terms of what makes up quality healthcare. According to Wallace and Jermy (2015:2517) quality in healthcare began during Florence Nightingale’s involvement as a nurse in the Crimean War utilising descriptive statistics to discover a positive correlation between unsanitary conditions and patient death.
Today, the Institute for Healthcare Improvement and Bill & Melinda Gates foundation Ethiopia, which was developed in 2010 is the leading organization in healthcare quality. The importance of quality can be stated in the following sentences – « No quality, no sales. No sale, no profit. No profit, no jobs ». The quality of health services provided by health providers is becoming more and more vital and the demands of quality control, managements and improvements (Behzad et al 2016:475).
Dimensions of service quality
Reliability – consistency of performer and dependability.
Responsiveness – willingness or readiness to provide service, timeliness.
Competence – possession of skills and knowledge required to perform the service.
Access – approachability and ease of contact.
Courtesy – politeness, respect, consideration for property, clean and neat appearance. Communication – educating and informing customers in language they can understand, listening to customers.
Credibility – trustworthiness, belief, is having customer’s best interest at heart.
Understanding – making an effort to understand the customer’s needs, learning thespecific requirements, providing individualized attention, recognizing the regularcustomers.
Security- freedom from danger, risk or doubt.
Tangibles- the physical evidence of service (facilities, tools and equipment).
Benefits gained by quality to a firm are positive company image, better competitive ability and increased market share (Institute of Medicine)
Factors influencing healthcare service quality
Quality in a healthcare is a production of cooperation between the patient and the healthcare provider in a supportive environment. Personal factors of the provider and the patient, and factors pertaining to the healthcare organization, healthcare system, and the broader environment affect healthcare service quality. Healthcare quality can be improved by supportive visionary leadership, proper planning, education and training availability of resources, employees and processes, and collaboration and cooperation among providers (Mosadeghrad 2014:85).
Table of contents :
Declaration
Abstract
Acknowledgements
Dedication
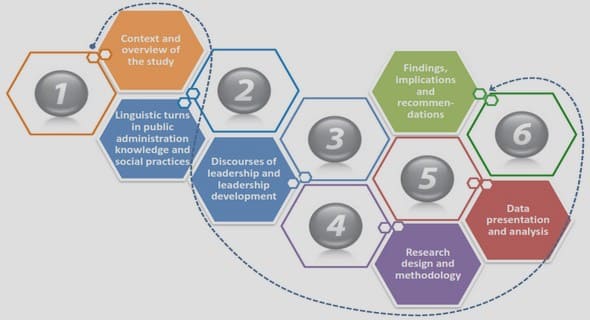
CHAPTER 1 ORIENTATION TO THE STUDY
1.1 INTRODUCTION
1.2 BACKGROUND TO THE RESEARCH PROBLEM
1.3 STATEMENT OF THE RESEARCH PROBLEM
1.4 RESEARCH PURPOSE
1.4.1 Research objectives
1.4.2 Research questions
1.5 DEFINITIONS OF TERMS
1.5.1 Assessment of quality.
1.5.2 Health centre
1.5.3 Health care provider satisfaction
1.5.4 Health service
1.5.5 Quality of care delivery
1.5.6 Primary Hospital.
1.6 THEORETICAL FRAMEWORK
1.6.1 Theoretical foundations of the study
1.7 SIGNIFICANCE OF THE STUDY
1.8 INTRODUCTION TO RESEARCH METHODOLOGY
1.8.1 The study context
1.9 SUMMARY
1.10 ORGANIZATION OF THE THESIS
CHAPTER 2 LITERATURE REVIEW
2.1 INTRODUCTION
2.2 DEFINITIONS OF QUALITY
2.2.1 Dimensions of quality
2.2.2 Dimensions of service quality
2.2.3 Factors influencing healthcare service quality
2.2.4 Quality assurance versus quality improvement
2.3 DONABEDIAN’S MODEL OF QUALITY CARE
2.4 QUALITY HEALTHCARE
2.4.1 Structure
2.4.2 Process
2.4.3 Outcomes
2.5 RELEVANCE OF THE THEORETICAL FRAMEWORK TO THIS STUDY
2.6 STANDARD OPERATING PROCEDURES FOR QUALITY ASSURANCE
2.6.1 Operational model for quality in health care
2.6.2 Equitable access to quality health services
2.6.3 Regulatory systems
2.6.4 Health and health related indicators in Ethiopia
2.7 OROMIA REGIONAL STATE
2.8 GINDABARAT DISTRICT
2.9 HEALTH SYSTEM AND HEALTH POLICY
2.9.1 Health System
2.9.2 Health service delivery
2.10 DIMENSIONS OF HEALTH WORKFORCE PERFORMANCE
2.11 SUMMARY
CHAPTER 3 RESEARCH DESIGN AND METHODS
3.1 INTRODUCTION
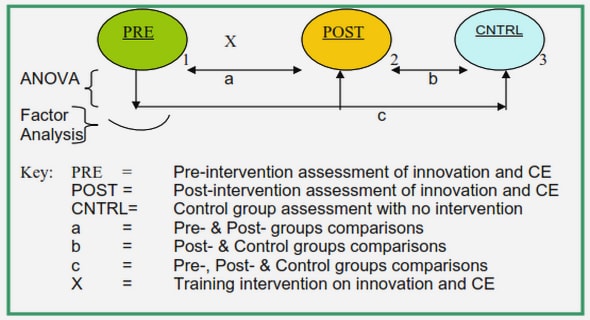
3.2 RESEARCH DESIGN
3.4 RESEARCH METHODS FOR PHASE 1
3.4.1 Study setting
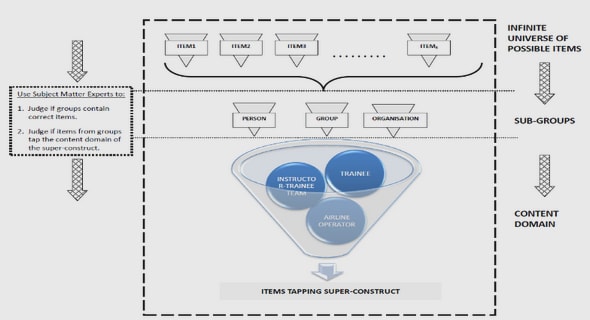
3.4.2 Population of the study
3.4.3 Sample and sampling methods
3.4.4 Ethical issues related to sampling
3.5 DATA COLLECTION
3.5.1 Development and testing of the data collection instrument
3.6 DATA COLLECTION PROCESS
3.6.1 Ethical considerations related to data collection
3.7 DATA ANALYSIS
3.8 INTERNAL AND EXTERNAL VALIDITY OF THE STUDY
3.9 TRUSTWORTHINESS
3.10 RESEARCH METHODS FOR PHASE 2
3.11 SUMMARY
CHAPTER 4 ANALYSIS, PRESENTATION AND DESCRIPTION OF FINDINGS
4.1 INTRODUCTION
4.2 PHASE 1 QUANTITATIVE APPROACH
4.2.1 Quantitative data management and analysis
4.2.2 Quantitative data presentation
4.2.3 Interpretation and discussion of quantitative data
4.3 SERVICE DELIVERY PRACTICE GAPS IDENTIFIED AT GINDABARAT PUBLIC HEALTH FACILITIES
4.3.1 Organization management and quality improvement services.
4.4 OUTCOME RELATED GAPS IDENTIFIED AT GINDABARAT PUBLIC HEALTH FACILITIES
4.5 PHASE 2 Qualitative approach
4.6 DATA MANAGEMENT AND ANALYSIS
4.7 QUALITATAIVE RESEARCH PRESENTATION
4.7.1 Demographic characterstics
4.8 THEMES AND SUB-THEMES
4.9 PRESENTATION AND DISCUSSION OF RESULTS
4.10 CONVERGENCE OF QUANTITATIVE AND QUALITATIVE FINDINGS
4.11 SUMMARY
CHAPTER 5 DEVELOPMENT OF THE GUIDELINE TO ENHANCE THE QUALITY OF HEALTH SERVICE DELIVERY
5.1 INTRODUCTION
5.2 DEFINITION OF GUIDELINES
5.3 PURPOSE OF THE GUIDELINE
5.4 SCOPE OF THE GUIDELINES
5.5 STEPS FOLLOWED IN THE DEVELOPMENT OF GUIDELINES
5.6 DEVELOPED GUIDELINES
5.7 VALIDATION OF THE GUIDELINES
5.8 SUMMARY OF GUIDELINE DEVELOPMENT
5.9 SUMMARY
CHAPTER 6 CONCLUSIONS, LIMITATIONS AND RECOMMENDATIONS
6.1 INTRODUCTION
6.2 CONCLUSIONS ON THE FINDINGS
6.3 CONTRIBUTIONS OF THE STUDY
6.4 LIMITATIONS OF THE STUDY
6.5 CONCLUSIONS
6.6 RECOMMENDATIONS
6.7 SUMMARY
REFERENCES
ANNEXURES