Get Complete Project Material File(s) Now! »
THE HUMAN PAPILLOMAVIRUS AND ITS LINK TO INTRAEPITHELIAL AND INVASIVE CERVICAL NEOPLASIA
HISTORICAL PERSPECTIVE
In 1907 the viral aetiology of common warts was established and first described by Giuseppe Ciuffo. It was only in the 1970s with the advent of molecular technology when HPV was studied in detail (Ciuffo, 1907; Meisles and Fortin, 1976). The transmission of the virus from man to man was determined by innoculation with a cell-free extract of wart tissue. Warts may infect several sites in the human body and can also infect several animal species. Rous and Beard (1935) reported the link between benign papillomas in rabbits and certain cancers. As molecular technology advanced it became possible to study the molecular link between papillomaviruses and cancer. Meisels and Morin (1981) further described the high prevalence of HPV and cervical dysplasia. De Villiers et al (1981) cloned the first genital human papillomaviruses. Zur Hausen (1982) also described the link between papillomaviruses and other lesions. HPV types 6 and 11 were described in association with benign condylomata acuminate. Subsequently, together with other investigators (Durst et al, 1983 and Boshart et al, 1984) HPV types 16 and 18 were cloned by zur Hausen and others from cervical cancers and the transcription of these HPV types in cervical cancers was confirmed. Since then many studies confirmed the link between papillomaviruses and cervical dysplasia or cancers. In 1988 zur Hausen reported that HPV types 16 and 18 were present in about 70% to 80% of high grade squamous intraepithelial and invasive cervical neoplasias. With the advent of recombinant DNA technology and molecular cloning, many HPV types were discovered. To date more than 150 HPV types have been reported (zur Hausen, 2000).
EPIDEMIOLOGICAL EVIDENCE LINKING HPV AND CERVICAN NEOPLASIA
The highest rates of HPV infection is after the onset of sexual activity usually in the 20-30 year age interval. In most women HPV infection is self-limiting and as much as 90% of women will clear HPV infections over a period of time. The median duration of high-risk HPV infections is about one year and few months for low-risk infections (Schiffman and Kjaer, 2003). In populations at high risk of HPV infection, a second peak of HPV infection has been reported among postmenopausal women (Herrero et al, 2000). Of the women who develop persistent infections only 2-3% will develop cervical dysplasia (Clarke and Chetty, 2002). Results from epidemiological studies showed a consistent link between cervical cancers, pre-cancers and papillomaviruses. These studies included case series, case-controlled and cohort studies. Of the more than 100 HPV types described, about 40 have been shown to infect the genital tract (Woodman et al, 2007). Since some of the early studies utilized non-amplified DNA hybridization techniques the results were inconsistent. The point prevalence of HPV infection ranges from 14% to 35% (Ho et al, 1998). Munoz et al (1988) reported a wide range of 15% to 92% of the presence of HPV DNA in cervical tumour specimens. However, with the advent of the highly sensitive polymerase chain reaction (PCR) technology, there emerged strong molecular evidence for the link between HPV and cervical neoplasias (Schiffman et al 1993; Munoz et al, 1992). The largest study of the prevalence of HPV in cervical cancers was the International Biological Study on Cervical Cancer which studied over 1000 women from many countries and utilized PCR technology (Bosch et al, 1995). This study reported a prevalence of 93%. A re-analysis of the specimens was performed and with the use of different primers the prevalence of HPV in cervical cancers increased to 99.7%. This high prevalence is consistent across the world even in areas of varying prevalence of cervical cancer and was demonstrated in both retrospective and prospective studies (Bosch, 2002).
Based on information pooled from 11 case-controlled studies (Munoz et al, 2003), it has been established that there are 15 high-risk HPV types which are oncogenic to the epithelium of the anogenital tract (16, 18, 26,31, 33, 35, 39, 45, 51, 52, 53,56, 58, 59, 66, 68, 73 and 82). Twelve types are regarded as low-risk HPV types (6, 11, 40, 42, 43, 44, 54, 61, 70, 72, 81 and CP6108). The oncogenicity of all other HPV types is unknown. HPV types 16 and 18 have been identified in about 70% of cervical carcinomas (Clifford, 2003). Across the world HPV types 16 and 18 predominate in cervical carcinomas (Clifford, 2005).
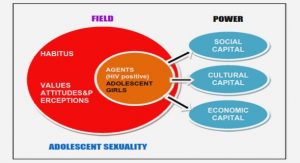
The sequence of events leading to the development of invasive cervical carcinomas was subsequently established. It became evident that HPV infection was a necessary factor followed by the development of intraepithelial lesions and then cervical carcinomas. Herrero et al (2000) demonstrated that HPV infection was acquired after sexual activity in young women. The prevalence of HPV infection then declined after the age of 30 years. Smith et al (2008) reported the age-specific prevalence of HPV in a meta-analysis of 346 160 women. It was noticed that HPV prevalence decreased with increasing age from peak prevalence in women younger than 25 years of age. In women between 25 and 35 years, the HPV prevalence differed in different geographical regions of the world from 15% in Northern Europe to 20% in Africa. In older women, there were inconsistent trends with a decrease or plateau noticed in most studies. Low-grade cervical squamous intraepithelial lesions (LGSIL) were commonest around the age of 29 and were associated with many HPV types. Its prevalence then declined after the age of 30 years. Low-risk HPV infection is associated with transient HPV types, whereas high-risk HPV types are associated with more persistent infections (Franco et al, 1995). High-risk HPVs are also associated with a greater risk of progression from atypical cells of undetermined significance (ASCUS) to high grade lesions and greater duration of infection compared to low-risk HPVs (Schlecht et al, 2003). High-grade cervical squamous intraepithelial lesions (HGSIL) were noted commonly between the age of 30 and 40 years. High-risk HPVs notably types 16 and 18 were dominant in HGSIL lesions and cervical cancers. The odds ratios described were 320 for HGSIL and 710 for cervical carcinomas. Sun et al (1997) reported that HIV-infected women have a higher incidence of high-risk HPV types in low-grade squamous intraepithelial lesions (LGSIL). Although about 60% of low-grade intraepithelial lesions regress in HIV non-infected women, this regression rate decreases to about 27% in HIV-infected women (Petry et al, 1994; Maiman et al, 1993). Langerhans cells are the antigen-presenting cells of the cervix. Spinillo et al (1993) reported a significant reduction in Langerhans cells in CIN lesions among HIV-infected women compared to a matched control group.
CLASSIFICATION AND STRUCTURE OF PAPILLOMAVIRUSES
Previously the Papillomaviruses belonged to the Papillomavirus genus and with the Polyomavirus genus, constituted the Papovaridae family. They are now grouped independently as the papillomavidae family and are unrelated to polyomaviruses and SV40. The size and genomic organization of the two genera are different. Animal papillomaviruses are species-specific and have a predilection for epithelia at specific sites. These viruses share structural and functional similarities, including the ability for proliferation and transformation of the host epithelium. They are associated with dysplastic and neoplastic processes. The HPVs exist in a number of types called genotypes since their classification is based on the nucleotide of which about 40 infect the anogenital epithelium.
The Papillomaviruses are classified according to the DNA sequence homology in certain genes, especially the L1 gene, which codes for the viral capsid. This classification has been ratified by the International Committee on the Taxonomy of Viruses (de Villiers et al, 2004). For a new HPV type to be confirmed, the total DNA from the virus must be cloned and the DNA sequence must be obtained from the E6, E7 and L1 genes. The L1, E6 and E7 genes of any type should have less than 90% identity with any other known type. A subtype is established if new isolates have a homology between 90 – 98% with any known type. A variant is established if a new isolate has more than 98% homology. Papillomaviruses which share a 60% homology in the L1 region are grouped together in the α and π genera. The α genus includes all high-risk HPVs, low-risk HPVs, whereas the papillomaviruses include viruses associated with Epidermodysplasia verruciformis. The genera are further sub-divided into species e.g., α9 includes 16, 31, 33, 35, 52 and 58. Depending on their tropism, they are divided into mucosal and cutaneous types. The phylogenetic tree representing the family of papillomaviruses is represented in Figure 1.
STRUCTURE OF THE HUMAN PAPILLOMAVIRUS
Human Papillomaviruses are small, double-stranded DNA viruses of about 55nm with an icosahedral protein capsid containing 72 capsomers. It has a circular genomic structure containing 7500 to 8000 base pairs.
The capsid has two structural proteins:
- The L1 protein which makes up 80% of the total viral protein with a molecular mass of 53 000 – 59000 daltons. This protein is the major capsid protein encoded by the L1 gene
- The L2 protein is a minor protein with a molecular weight of 70 000 daltons and is encoded by the L2
THE HPV NUCLEIC ACID/GENOME
Within the capsid is the circular double-stranded supercoiled DNA genome of approximately 8 kilobases (Kb) in length with a molecular weight of 5 X 10 6 daltons. Only one strand of this genetic material serves as a template for DNA transcription or open reading frames (ORFs) (Cole et al, 1987). The genome is divided into early (E), late (L) and non-coding regions. The open reading frames are the coding regions and are classified as “early” or “late” depending on when gene function occurs in a specific time period in the life-cycle of the HPV infection. Early genes are expressed at the onset of the infection and mediate specific gene functions which control viral DNA transcription, replication and cellular transformation. The E1 and E2 genes play a role in viral replication and maintenance of the genome. The linear representation of the HPV genome is represented in Figure 2.
CHAPTER ONE INTRODUCTION
1.0 EPIDEMIOLOGY OF CERVICAL CANCER
1.1 RISK FACTORS AND AETIOLOGY OF CERVICAL CANCER AND IT’S PRECURSORS
1.1.1 PARITY
1.1.2 THE NUMBER OF SEXUAL PARTNERS AND FREQUENCY OF SEXUAL INTERCOURSE
1.1.3 SMOKING
1.1.4 ROLE OF THE MALE PARTNER
1.1.5 ROLE OF DIETARY FACTORS
1.1.6 ROLE OF SEXUALLY TRANSMITTED INFECIONS OTHER THAN HPV
1.1.7 ROLE OF THE HUMAN IMMUNODEFICIENCY VIRUS (HIV) INFECTION
2.0 THE HUMAN PAPILLOMAVIRUS AND ITS LINK TO INTRAEPITHELIAL AND INVASIVE CERVICAL NEOPLASIA
2.1 HISTORICAL PERPECTIVE
2.2 EPIDEMIOLOGICAL EVIDENCE LINKING HPV AND CERVICAL NEOPLASIA
2.3 CLASSIFICATION AND STRUCTURE OF PAPILLOMAVIRUSES
2.4 STRUCTURE OF THE HUMAN PAPILLOMAVIRUS
2.5 THE HPV NUCLEIC ACID/GENOME
2.5.1 ORFs WITH ONCOGENIC PROPERTIES
2.5.2 REGULATORY GENES
2.5.3 UNKNOWN GENE FUNCTIONS
2.5.4 LATE CAPSID PROTEINS AND THE UPSTREAM REGULATORY REGION
2.6 REPLICATION CYCLE OF THE HUMAN PAPILLOMAVIRUS
2.7 IMMUNOLOGY OF HPV INFECTIONS
3.0 CLINICAL CORRELATES OF HPV TYPES
3.1 CUTANEOUS HPVs IN IMMUNO-COMPETANT POPULATION
3.2 CUTANEOUS HPVs IN IMMUNO-COMPROMISED INDIVIDUALS
3.3 HPVs AFFECTING THE AERO-DIGESTIVE AND ANOGENITAL MUCOSAE
4.0 VULNERABILITY OF THE HOST TO CERVICAL NEOPLASIA
4.1 THE CELL CYCLE AND ITS ASSOCIATION WITH HUMAN PAPILLOMAVIRUS INFECTION
4.2 CELL-CYCLE PROTEINS
5.0 THE ROLE OF HPV IN RELATION TO THE CELL CYCLE
6.0 THE p53 GENE AND ITS ROLE IN CERVICAL CANCER
6.1 HISTORY
6.2 THE p53 GENE AND CERVICAL CANCER
7.0 THE ROLE OF TELOMERASE ACTIVITY IN HPV-RELATED CERVICAL CANCER
8.0 THE ROLE OF DNA METHYLATION IN CERVICAL CANCER
9.0 MICROSTAELLITE INSTABILITY AND CERVICAL CANCER
10.0 THE ROLE OF STEROID CONTRACEPTION, HUMAN PAPILLOMAVIRUS AND CERVICAL NEOPLASIA
10.1 INTRODUCTION
10.2 THE BENEFITS OF STEROID CONTRACEPTION
10.3 CANCERS LINKED TO STEROID CONTRACEPTION
10.4 REVIEW OF PUBLISHED DATA LINKING STEROID CONTRACEPTION TO CERVICAL NEOPLASIA
11.0 POSTULATED MECHANISMS OF STEROID-RELATED CERVICAL CARCINOGENESIS AND THE LINK BETWEEN STEROID CONTRACEPTION AND HUMAN PAPILLOMAVIRUS nINFECTION
12.0 THE IMPLICATIONS OF THE EVIDENCE PROVIDED FOR CLINICAL PRACTICE WITH REGARDS TO STEROID CONTRACEPTION
13.0 HPV VACCINES AND THE FUTURE
14.0 PART ONE OF THE PROJECT
14.1 AIMS
14.2 PATIENTS AND METHODS
14.3 STATISTICAL METHODS
14.4 RESULTS
14.5 DISCUSSION
15.0 PART TWO OF THE PROJECT
15.1 HYPOTHESIS OF THE STUDY
15.2 AIMS
15.3 MATERIALS AND METHODS
15.4 LABORATORY METHODS
16.0 STATISTICAL METHODS
17.0 RESULTS
17.1 PATIENT DEMOGRAPHICS
17.2 CLINICAL DATA
17.3 CONTRACEPTIVE DATA
17.4 SMOKING
17.5 RNA EXTRACTION
17.6 HISTOLOGY FOR 63 PATIENTS
17.7 CLINICAL STAGES FOR 63 PATIENTS
17.8 EXPRESSION OF HPV 16 E6, E6*I& E6*II ONCOGENES FOR 63 PATIENTS
17.9 CLINICAL STAGE VERSUS HPV 16 E6 ONCOGENE EXPRESSION
17.10 EXPRESSION OF THE HPV TYPE 16 E6*I/E6*II ONCOGENES IN STEROID USERS AND NON-STEROID USERS
17.11 EXPRESSION OF THE HPV 16 E6*I/E6*II IN RELATION TO STAGE
18.0 DISCUSSION
19.0 CHAPTER FIVE
19.1 CONCLUSIONS AND RECOMMENDATIONS
20.0 APPENDIX
21.0 REFERENCES
GET THE COMPLETE PROJECT