Get Complete Project Material File(s) Now! »
Barriers
Wootton et al. (2006) identify a number of barriers associated with telemedicine, such as the quality of health information delivered and the breakdown in relationships between health professionals, and health professionals and patients.
Furthermore, there was concern over difficulties within the organisations with bureaucracy. McCrossin (2003) identified barriers such as planning and executive failure. Executive failure arises when the plan is sufficient, or when the actions taken do not follow the plan. Additionally, planning failure is when the plan is inadequate. Joseph, West, Shickle, Keen, and Clamp (2011) and Stronge et al. (2007) identified challenges in implementing telemedicine, naming staff scepticism and training as key. A lack of dedicated project management and recurrent funding issues were considered to be limitations of successful implementation. Care should be taken in an uncertain climate, such as healthcare, when introducing new methods of service such as telemedicine, as people usually favour the already known (McCrossin, 2003). Furthermore McCrossin (2003) suggests men are generally disbelieving of new things unless they have been well tested by experience. When introducing telemedicine Buck (2009) and Stronge et al. (2007) suggest it is important to first consider the needs of the user, as success depends on the interaction between the user and the technology. Furthermore, Buck (2009) suggests that in order for telemedicine to be accepted the user must immediately understand what added value it will give and why it exists.
Doctors’ perception of the usefulness of telemedicine was found to be a contributing factor of doctors acceptance of the tool (Buck, 2009). Recruiting the right patients and having technology that was compatible with telephone systems can be a challenge and in one study none of the organisations had long term strategic plans for telemedicine (Stronge et al., 2007).
Although mentioned in the previous section as a driver, technology can in fact be a barrier to telemedicine. The paper by Pryke (2012) suggests a problem when trying to utilize technology with the elderly, as there are still many elderly living in rural and remote areas that suffer from IT illiteracy.
In NZ there are 21 individual District Health Boards (DHB) with a population of nearly 4.5 million (Statistics New Zealand, 2012b). Many DHBs have clinical information systems and networks that are not compatible with other healthcare providers, in some cases in the same regions. Slow video access, poor picture quality and delay in sound have added to the struggle of integrating telemedicine into Emergency Departments (Parker, 2005). Moreover, staff in Emergency Departments work in a “fast paced environment were activity requires flexibility” (p. 70), and the perception is telemedicine technology will not lend itself to the diversity and pace needed. A report by Giordano, Clark, and Goodwin (2011) from Scotland recognises there are a number of lessons to learn when adopting telemedicine, such as ensuring that professionals are prepared to work differently as individual caseloads will not increase otherwise. Furthermore, ensuring that the service needs are met by the technology requires proper analysis of how the model of care should look prior to buying equipment from vendors. If this is not done then the waste of expensive costly equipment can occur by underuse or no use at all (Parker, 2005).
Chapter One: Introduction
Introduction
Aim of the study
Background:
Personal background
Language
Structure of the thesis
Summary
Chapter Two: Literature Review .
Introduction
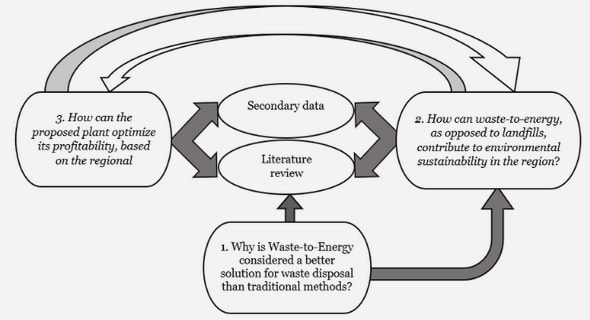
Process for Literature review
Definitions
History
Drivers of telemedicine
Non Technological Drivers .
Technological Drivers
Barriers
Opportunities
Chapter Three: Methods of research
Introduction
Aim of the Research
Timeline for the study
Background
Research Methodology
Design of research .
Data Collection
Data analysis
Summary
Chapter Four: Findings from NZ Interviews
Introduction .
Participants
Themes
Implementation
Skills
Opportunities
Barriers
Chapter Five: Queensland Australia
Chapter Six: Discussion
Chapter 7: Conclusion
Appendices .
GET THE COMPLETE PROJECT
Clinicians’ Perceptions of Telemedicine: Opportunities and Barriers for Emergency Medicine