Get Complete Project Material File(s) Now! »
Comparison of predictive value of model with and without HbA1c
When considering the categorical NRI, 12%, 4%, and 9% of patients will be down-classified to being at low risk of GDM at 10, 50, and 100% respectively, by adding the HbA1c to the model. Similarly, 0%, 4%, and 0% will be up-classified to being at high risk of GDM at 10, 50, and 100% respectively when HbA1c was added to the model. The integrated discrimination improvement (IDI) shows that the discrimination slope of the updated model with the added HbA1c was 10.8% higher than the original model. The le Cessie – van Houwelingen – Copas – Hosmer unweighted sum of squares test for global goodness of fit for the model with HbA1c gave a p value of 0.87 and for the model without HbA1c 0.81.
Nomograms (a) with HbA1c and (b) without HbA1ca
The efficacy of the nomograms at >10% and >15% probabilities of GDM was then compared (Table 3) as the cut-off risk above which a woman is deemed at high risk of developing GDM had to be established. At a cut-off of 10%, 58/554 (10.5%) and 50/554 (9.0%) fewer OGTTs would be carried out if HbA1c was or was not incorporated into the nomogram, respectively. Two (0.4%) and one (0.2%) cases of GDM would be missed if the nomogram with and without the HbA1c was applied, respectively. Similarly, at a 15% cut-off 124/554 (22.4%) and 103/554 (18.6%) fewer OGTTs would be carried out if HbA1c was or was not incorporated into the nomogram, respectively. Nine (1.6%) cases of GDM would be missed whether or not HbA1c was incorporated into the nomogram.
Discussion
This study aimed to evaluate the use of risk indicators to develop a statistical prediction model for GDM. Traditionally identified risk factors such as BMI, age, or family history of diabetes mellitus have been associated with GDM in other populations. [21-24] Data on GDM in Africa, especially since the introduction of the FIGO criteria is scant. Available data found an association with GDM and obesity, family history of diabetes mellitus, previous stillbirth, previous macrosomic child and age >30 years in some sub-Saharan African populations. [23]
The fasting glucose appears to be a very attractive tool for screening pregnant women for GDM. However, all pregnant women would have to present in a fasted state for screening, thus this approach can only take place on the second antenatal visit, and would require all pregnant women to be tested. While this approach may not seem unrealistic, it can prove to be challenging in a low income country where women have to travel a great distance to the healthcare facility and they often do not have funds for transport. Thus an alternate screening tool that could be used easily on the first antenatal visit to stratify a women’s risk for GDM in the current pregnancy was investigated.
It was found that a previous history of delivering a baby weighing ≥4000 g and an elevated random blood glucose were independent predictors of developing GDM. Church et al. [25] and Meek et al. [26] found that the random glucose was a promising screening tool for GDM with AUROC of 0.8 and 0.86 respectively. By comparison these retrospective studies employed a 2-stage screening protocol for GDM and did not use the currently widely accepted FIGO diagnostic criteria. However, by comparison the basal random glucose alone was a poor predictor of women likely to develop GDM in our study. Thus it was proposed that this nomogram-based scoring system, by adding other variables to the random blood glucose, will better identify women at risk at GDM compared to the random blood glucose alone. This premise requires prospective validation of the nomogram in a real-world setting.
Other studies have also identified risk factors. [18, 19, 21-24] Only nine of these studies summarised the significant risk factors into a score or a clinical prediction model, of which eight (8) were tested on our study population (Table 4). These tests performed poorly as a screening tool in our study population compared with their derivation populations. This poor performance may be a result of testing these scores on a low risk pregnant population. Risk factors may play a less significant role in predicting GDM when universal screening is applied and the FIGO diagnostic criteria are used. By contrast most of the afore-mentioned scoring systems used a selective screening approach and used criteria other than that recommended by FIGO for the diagnosis of GDM in the derivation and the validation of their scores. [7-14] Furthermore, many of these scores use logarithmic equations in their calculations, thus necessitating a computer in the clinic, which is not always available in South African antenatal clinics.
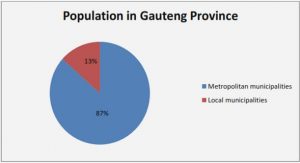
As South Africa is a resource-restricted country that faces a dual burden of disease, i.e. communicable and non-communicable diseases, a selective screening approach is an attractive option for the diagnosis of GDM as it seems the more cost effective approach. As a risk-factor based approach performs inconsistently, a scoring system that incorporates the more significant risk factors in a population may be a better option. Thus, a nomogram that incorporates the significant factors in a South African population was proposed. The BMI and history of previous deliveries are currently part of routine antenatal practice. The random blood glucose can easily be tested at the first antenatal visit, making the random glucose a clinically applicable tool for early in pregnancy. In some settings an HbA1c may be available. However, it was demonstrated that including the HbA1c into the risk stratification tool does not significantly influence the patients’ risk of GDM. South Africa has a high burden of HIV. In our study HIV did not influence the incidence nor did it contribute as a predictive marker of GDM.
Chapter 1
Introduction
Chapter 2
Screening for gestational diabetes in a South African population: prevalence, comparison of diagnostic criteria and the role of risk factors
Chapter 3
Selective screening strategies for gestational diabetes, a prospective cohort observational study
Chapter 4
Evaluating the utility of a point-of-care glucose meter for the diagnosis of gestational diabetes
Chapter 5
Association between gestational diabetes and biomarkers: A role in diagnosis
Chapter 6
Summary and Recommendations
Appendix A
Ethics Approval
Appendix B
Questionnaire