Get Complete Project Material File(s) Now! »
INTRODUCTION
Craniofacial anomalies (CFA) are the fourth most common birth anomalies that occur in approximately 1 in 700 live births (ACPA, 2007: 5; Peterson-Falzone, Hardin-Jones & Karnell, 2010: 15; WHO, 2002: 10). Cleft lip and/or palate (CL/P) is the most common type of CFA and it affects all races across worldwide. The exact cause of CL/P is not known but it is linked to environmental influences, genetic factors and gene-environment interaction (Peterson-Falzone et al., 2010: 38; Watson, Sell & Grunwell, 2001: 10; Wyszynski, 2002: 283). The CL/P causes a pervasive impact on speech, hearing, appearance and cognition. This has a prolonged and adverse influence on the health and social integration of an individual with CL/P.
There are considerable costs of cleft care in terms of health care, emotional disturbance, and social and employment factors impacting individuals with CL/P, their families and society on the whole (WHO, 2002: 2). The management of CL/P involves a multidisciplinary approach and most developed countries have well established protocols for cleft care. The American Cleft-Palate Craniofacial Association (ACPA, 2007), the Eurocran Speech Project (2000) and the World Health Organization (WHO, 2002), have emphasized the need for a well-coordinated, effective team- based approach and early intervention programmes. However, there are numerous challenges to providing cleft care in resource limited developing countries.
It is estimated that 80% of the population of individuals with clefts live in the developing or less developed world and may not receive adequate cleft care (Mars, Sell & Habel, 2008: 1). The surgical team is at the core of management of CL/P in most countries. However, role of the speech-language therapists and audiologists in providing cleft care is not well established in countries with limited resources. It is well recognised that children with CL/P are at risk of communication delays/disorders (ACPA, 2007: 5; Peterson-Falzone, Trost-Cardamone, Karnell & Hardin-Jones, 2006: 9; Rossetti, 2001:3; Strauss, 2004: 150). Early identification and management of communication difficulties by a speech-language therapist and audiologist has a positive impact on the child’s overall development (Billeaud, 2003: 53; Bzoch, 2004: 19; Rossetti, 2001: 267; Scherer, D’Antonio & McGahey, 2008: 30).
The number of speech- language therapists and audiologists in developing countries is limited (D’Antonio & Nagarajan, 2003: 308). As a result there is a lack of awareness of their contribution to cleft services. These factors clearly indicate a need to establish the roles of speech-language therapists and audiologists at an early stage in the management of CL/P. In acknowledgement of the many challenges to cleft care in developing countries, clinicians and researchers are currently focusing their attention towards global strategies for improved cleft care. The WHO (2002: 33) recommended international research collaborations and guidelines to improve clinical practice. However, local needs for the cleft care are likely to vary, thus clinical decision-making in speech-language therapy should be guided by research evidence, as recommended by Reilly (2004: 115). International collaboration is a prerequisite for research into the etiology, prevention and treatment of cleft lip and palate.
A critical mass of clinical researchers including epidemiologists and basic scientists is required to generate comprehensive research evidence (WHO, 2002: 2). In order to facilitate international collaboration it is recommended that a set of guidelines for the provision of clinical services and the maintenance and analysis of minimum clinical records are adopted internationally (WHO, 2001b: xi). Developing countries invariably face economic constraints in complying with these recommendations; however, the guidelines should serve as long-term desirable goals in providing an optimal standard of cleft care.
TABLE OF CONTENTS :
- ABSTRACT
- OPSOMMING
- CHAPTER 1: INTRODUCTION AND ORIENTATION
- 1.1 INTRODUCTION
- 1.2 OVERVIEW OF INTERVENTIONS FOR YOUNG CHILDREN WITH CLEFT LIP AND/OR PALATE IN DEVELOPING AND DEVELOPED COUNTRIES
- 1.3 STATEMENT OF THE PROBLEM
- 1.4 RATIONALE FOR THE STUDY
- 1.5 THE RESEARCH APPROACH
- 1.6 TERMINOLOGY
- 1.7 ABBREVIATIONS
- 1.8 ORGANISATION OF THE STUDY
- 1.9 CONCLUSION
- 1.10 SUMMARY
- CHAPTER 2: CLEFT CARE PRACTICES FOR YOUNG CHILDREN
- 2.1 INTRODUCTION
- 2.2 IMPACT OF A CLEFT ON A YOUNG CHILD AND THE FAMILY
- 2.2.1 Impact of a cleft on communication development
- 2.2.2 Impact of a cleft on general development
- 2.2.3 Impact of a cleft on parents and families
- 2.3 RECOMMENDED BEST PRACTICE FOR THE CARE OF YOUNG CHILDREN WITH CLEFT LIP AND/OR PALATE
- 2.3.1 Team approach
- 2.3.2 Early communication intervention and parental participation
- 2.3.3 Treatment outcome measures
- 2.3.4 National registry and databases for individuals with craniofacial anomalies
- 2.4 CONCLUSION
- 2.5 SUMMARY
- CHAPTER 3: COMMUNICATION ASSESSMENT OF YOUNG CHILDREN WITH CLEFT LIP AND/OR PALATE
- 3.1 INTRODUCTION
- 3.2 PURPOSES OF COMMUNICATION ASSESSMENT
- 3.3 RATIONALE FOR A NEW COMMUNICATION ASSESSMENT PROTOCOL IN A DEVELOPING COUNTRY
- 3.4 AREAS OF COMMUNICATION ASSESSMENT AND DEVELOPMENTAL ASSESSMENT STAGES
- 3.4.1 Case history
- 3.4.2 Genetic screening
- 3.4.3 Feeding
- 3.4.4 Hearing and listening skills
- 3.4.5 Communication interactions, pragmatics and speech-language development
- 3.4.6 Emergent literacy skills
- 3.4.7 Orofacial structures and oral motor function
- 3.4.8 Speech production
- 3.4.9 General developmental screening
- 3.5 ASSESSMENT PROCEDURES AND INSTRUMENTS FOR YOUNG CHILDREN WITH CLEFT LIP AND / OR PALATE
- 3.5.1 Procedures for case history taking
- 3.5.2 Genetic screening
- 3.5.3 Feeding assessment
- 3.5.4 Hearing and listening evaluations
- 3.5.5 Assessment of communication interactions, pragmatics and speech-language development
- 3.5.6 Emergent literacy skills’ assessment
- 3.5.7 Orofacial examination
- 3.5.8 Speech production assessment
- 3.5.8.1 Perceptual speech assessment procedures
- 3.5.8.2 Instrumental speech assessment procedures
- 3.5.9 Developmental screening
- 3.6 CHALLENGES TO COMMUNICATION ASSESSMENT IN DEVELOPING COUNTRIES AND POSSIBLE SOLUTIONS
- 3.7 CONCLUSION
- 3.8 SUMMARY
- CHAPTER 4: METHODOLOGY
- 4.1 INTRODUCTION
- 4.2 CONCEPTUAL FRAMEWORK
- 4.3 RESEARCH AIM AND OBJECTIVES
- 4.4 RESEARCH DESIGN AND THE RESEARCH PHASES
- 4.5 CONTEXT OF THE STUDY
- 4.6 RESEARCH ETHICS
- 4.7 PHASE ONE
- 4.7.1 Objectives of Phase One
- 4.7.2 Phase One participants
- 4.7.2.1 Children with cleft lip and/or palate
- 4.7.2.2 Parents of the children as respondents
- 4.7.2.3 Speech-language therapists and audiologists as participants
- 4.7.3 Phase One materials
- 4.7.3.1 Hospital medical records
- 4.7.3.2 Interview schedule
- 4.7.4 Phase One data collection procedure
- 4.7.5 Phase One data recording and analysis
- 4.7.6 Phase One validity and reliability
- 4.8 PHASE TWO
- 4.8.1 Objectives of Phase Two
- 4.8.2 Phase Two participants
- 4.8.2.1 Children with cleft lip and/or palate
- 4.8.2.2 Speech-language therapists and audiologists
- 4.8.2.3 Additional support staff
- 4.8.3 Phase Two materials and apparatus
- 4.8.3.1 Compilation of the Communication Assessment Protocol
- 4.8.3.2 Compilation of the speech material
- 4.8.3.3 Questionnaire: Perceptions of the speech-language therapists and audiologists regarding the Communication Assessment Protocol
- 4.8.4 Phase Two pilot study
- 4.8.4.1 Objectives of the pilot study
- 4.8.4.2 Pilot study participants
- 4.8.4.3 Pilot study materials and apparatus
- 4.8.4.4 Training of the speech-language therapists and audiologists
- 4.8.4.5 Pilot study data collection procedure
- 4.8.4.6 Pilot study results
- 4.8.5 Phase Two data collection procedure
- 4.8.6 Phase Two data analysis
- 4.8.7 Phase Two validity reliability and trustworthiness
- 4.9 PHASE THREE
- 4.9.1 Objectives of Phase Three
- 4.9.2 Phase Three participants
- 4.9.2.1 Speech-language therapists and audiologists
- 4.9.2.2 Additional support staff
- 4.9.3 Phase Three materials and apparatus
- 4.9.3.1 Data collection instrument: Questionnaire
- 4.9.3.2 Focus group topic guide
- 4.9.3.3 Apparatus
- 4.9.4 Phase Three data collection procedure
- 4.9.4.1 Self-administered questionnaire
- 4.9.5 Phase Three data analysis
- 4.9.6 Phase Three validity, reliability and trustworthiness
- 4.10 CONCLUSION
- 4.11 SUMMARY
- CHAPTER 5: RESULTS AND DISCUSSION
- 5.1 INTRODUCTION
- 5.2 BACKGROUND INFORMATION
- 5.2.1 Background information of the children with CL/P in the sample
- 5.2.2 Family characteristics and home languages of the children
- 5.2.3 Parental perceptions of feeding, speech and hearing problems in children with CL/P
- 5.3 CHARACTERISTICS OF THE CHILDREN WITH CLEFT LIP AND/OR PALATE BASED ON THE COMMUNICATION ASSESSMENTS
- 5.3.1 Feeding
- 5.3.2 Hearing abilities
- 5.3.3 Orofacial characteristics
- 5.3.4 Communication, speech and language characteristics
- 5.3.5 Emergent literacy skills
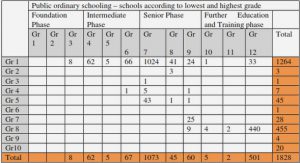
- 5.3.6 Developmental and educational aspects
- 5.4 CLINICAL APPLICABILITY OF THE COMMUNICATION ASSESSMENT PROTOCOL
- 5.4.1 Identification of communication disorders using the Communication Assessment Protocol
- 5.4.2 Reliability of the auditory perceptual speech analysis
- 5.5 CLINICAL ACCEPTABILITY OF THE COMMUNICATION ASSESSMENT PROTOCOL
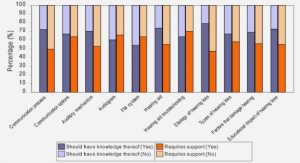
- 5.5.1 Speech-language therapists’ and audiologists’ perceptions as obtained by the questionnaire
- 5.5.2 Speech-language therapists’ and audiologists’ perceptions shared in the focus group discussion
- 5.6 CONCLUSION
- 5.7 SUMMARY
- CHAPTER 6: CONCLUSIONS AND IMPLICATIONS
- 6.1 INTRODUCTION
- 6.2 SYNOPSIS OF THE PREVIOUS CHAPTERS
- 6.3 CRITICAL REVIEW OF THE STUDY
- 6.3.1 Strengths of the study
- 6.3.2 Limitations of the study
- 6.4 CONCLUSIONS
- 6.5 IMPLICATIONS OF THE RESEARCH
- 6.6 RECOMMENDATIONS FOR FUTURE RESEARCH
- 6.7 FINAL COMMENTS