Get Complete Project Material File(s) Now! »
Impact of precursor frequency and diversity
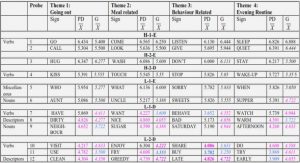
Direct measurements of Ag-specific populations in mice have shown that the size of Ag-specific inexperienced populations vary in a predictable fashion, with significant differences among distinct epitopes, but highly conserved frequencies among individuals that express at least one similar MHC allele. The impact of such variations on later immune responses is key, and has been investigated in mice. Early (<1 week) after peptide immunization, whatever the dose of peptide utilized, there is a positive correlation between pre- and post- immunization CD4+ T cell frequencies (Figure 9A). Similar observations were reported for CD8+ T cells, but when precursor frequencies are significantly different (>5-fold) (Kotturi et al., 2008; Obar et al., 2008). Besides magnitude, T cell precursor frequency was also demonstrated in mice as a key factor for early kinetics (an increased precursor frequency resulting in a more rapid response), and immunodominance hierarchy (Kotturi et al., 2008; Lo et al., 2014; Obar et al., 2008). It also predicts qualitative aspects of the memory T cell response, with increased precursor frequencies translating into rapid acquisition of a CD62Lhi central-memory phenotype (Obar et al., 2008). Finally, precursor frequencies is a mode of virus escape in LCMV model of infection (Kotturi et al., 2008). In humans, the same impact of precursor frequency on the magnitude and immunodominance patterns of responses were found in studies of influenza-infected humanized HLA-transgenic mice (Tan et al., 2011), HCV-specific peripheral T cells (Schmidt et al., 2011), and B.anthracis-vaccinated individuals (Kwok et al., 2012).
It is important to consider that some studies on mice infected with influenza (Cukalac et al., 2014; La Gruta et al., 2010), or Respiratory Syncytial Virus (RSV) (Ruckwardt et al., 2011) did not confirm the « precursor frequency to magnitude » correlation. One possible explanation for this discrepancy is that the impact of precursor frequency will only manifest in situations where the other parameters that influence immunodominance are controlled and comparable. This includes efficiency of antigen processing and presentation, MHC binding properties, epitope abundance at the surface of presenting APCs, viral load and kinetics of viral protein expressions. Alternatively, qualitative properties of the initial Ag-specific population, such as the proportion of high-affinity T cells, might influence its behavior after immunization (Cukalac et al., 2014). In other words, the work presented above has now established precursor frequency as a crucial factor in shaping adaptive immune responses, but qualitative parameters must also be taken into account when trying to predict the effective epitopespecific response after antigenic challenge (Jenkins and Moon, 2012). In particular, each of the subsets identified as part of the T cell inexperienced populations (as reported in Table 3) has a specific threshold for TCR activation and sensitivity to cytokine signals, and a specific pattern of function. RTEs and CD5hi NP cells have increased threshold for TCR activation (Berkley et al., 2013; Dalloul, 2009). Inversely, MP cells are hyperresponsive when encountering their cognate antigen (Haanen et al., 1999; Lee et al., 2013; Younes et al., 2011). However, how much the proportion of each of these subsets inside a given Ag-specific population influences the global behavior of that population during homeostasis and after immunization is unknown (Figure 9B).
HCV as a model of chronic inflammation
Hepatitis literally means inflammation of the liver. It can be acute or chronic, symptomatic or not, and relate to many different causes. Viral hepatitis is the leading cause worldwide, and refers to infection with one of the five hepatotropic viruses A, B, C, D and E. Major characteristics are summarized in Our laboratory focuses on chronic infection with the hepatitis C virus (HCV), because it is a major public health problem, and a leading cause of primary liver cancer. HCV naturally trigger an immunemediated inflammatory response (hepatitis) that is either:
• acute, self-limited, and beneficial – leading to clearance of the infection in about one-third of the patients.
• chronic, systemic and deleterious – slowly destroying the liver and possibly leading to extrahepatic manifestations, including extra-hepatic carcinogenesis.
Treatment and clearance benefits
HCV is to date the only chronic viral infection that can be cured. Curing is achieved by induction of a Sustained Virologic Response (SVR) by appropriate treatment. Sustained virologic responders (SVRs) – i.e. patients achieving SVR, are individuals with no detectable virus in the serum 3-6 months after the end of the treatment. It probably correspond to complete eradication of the virus from the blood, the liver, and any potential other reservoir. Indeed, after SVR, reappearance of the virus never happens, even when patients later undergo severe immunosuppression (e.g. chemotherapy or organ transplantation).
In the 80’s, patients were initially treated with subcutaneous injections (SC) of alpha-interferon (IFN α). It acts both directly on the virus, and indirectly by immuno-modulating the cellular immune response, reinforcing the endogenous interferon naturally present in response to HCV. It cured only 6- 12% of patients after 6 months. Extension to 12 months increased prolonged response to 16-20%. In the 90’s, a nucleosidic analogue – ribavirine (RBV), was proposed in association with IFNα. Also it had no effect in monotherapy, it permitted to double virological efficacy when associated to IFNα administration. Its mechanism of action is uncertain, but is likely multiple, with (i) immunomodulation in favor of Th1 lymphocytes; (ii) incorporation into the viral genome – thus limiting its replication; (iii) direct inhibition of viral polymerase NS5B; (iv) mutagenesis during viral replication; and (v) modulation of IFN-induced gene expression (Feld and Hoofnagle, 2005). Development of pegylated interferon (peg-IFNα) permitted to reduce the number of SC to 1 per week. Combination of peg-IFNα and RBV (800 mg/day for genotypes 2 or 3, or adapted to the weight [13-15 mg/kg/day] for genotypes 1 or 4) was for long the reference treatment. It permits clearance of the virus in 45% of genotype 1, 85 % of genotype 2, 70 % of genotype 3, 65 % of genotype 4, and 75% of rare genotypes 5 and 6. Factors influencing duration and modality of treatment are viral genotype, initial viremia, presence of extensive fibrosis or cirrhosis, IL28B genotype, response to a previous treatment, and viral kinetic at 4 and 12 weeks of treatment. Typically, patients are treated 24 (genotype 2 and 3) to 48-72 weeks (genotype 1, 4, 5).
With improved knowledge on the cell cycle of HCV, direct acting antiviral agents (DAA) have been recently developed (Pol et al., 2013) (Figure 12). First molecules in 2011 were inhibitors of NS3/NS4A protease (telaprevir and boceprevir). Association of these molecules to peg-IFNα and RBV permitted to increased SVR to 75 % in genotype 1 naive patients, and is the recommended treatment for genotype 1 patients, especially those at risk of non responding to classical bitherapy. However, protease inhibitors can lead to serious secondary events such as cutaneous eruptions, or
severe anemia in 49% of treated patients. Also, these treatments are expensive – 35 000 euros for one tritherapy, and thus not affordable worldwide. Since then, other direct molecules have been developed: second generation of proteases inhibitors, nucleos(t)idic or non nucleos(t)idic polymerase NS5B inhibitors, and inhibitors of the NS5A replication complex. The current interferon-free oral combinations allow more than 90% of cure for all patients. The main limitation remains their cost, estimated between 40 000 to 75 000 euros per individual.
HBV as a comparative model of chronic hepatitis
The hepatitis B virus is a DNA virus composed of a nucleocapsid core (HBc Ag) surrounded by an outer lipoprotein coat (envelope) containing the hepatitis B surface antigen (HBs Ag) (Table 4). It replicates via reverse transcription of a pregenomic RNA (pgRNA). Similar to HCV, HBV virus is hepatotropic, non cytopathogenic, and a major public health problem. Indeed, 350 millions persons are currently infected with HBV worldwide, with high risk of developing severe liver disease – chronicity, cirrhosis, liver failure and hepatocellular carcinoma (HCC), like in chronic HCV infection. After acute infection, 95% of infected adults clear spontaneously the HBV virus – but only 1% in the case of vertical transmission from mother to neonate. This is a major difference with HCV infection, where spontaneous clearance happens in 1/3 of patients whatever their age. Schematically, chronic
HBV infection evolves through three immune phases (Figure 18):
• immune tolerant (IT): HBe Ag+, HBV DNAhigh, ALT normal .
• immune clearance, or immunoactive (IA): HBe Ag+, HBV DNAhigh, ALT elevated, clinical symptoms .
• inactive chronic carrier (ICC): HBe Ag-, HBV DNAlow, ALT normal.
HBe Ag is a viral protein that is secreted by the HBV-infected cells. It is associated with chronic HBV infections. HBe Ag positivity is a marker of active viral disease and infectiousness. However, rare cases of e-Ag negative virus mutations can lead to false negativity of HBe Ag, and to misinterpretations.
Effector and resident memory T cells trafficking
After activation, effector CD8+ T cells downregulate LN-homing CD62L and CCR7 and start expressing chemokine receptors such as CXCR3, CCR5, CXCR6, CCR6, CXCR1, and CX3CR1. These induced chemokine receptors mediate effector CD8+ T cell migration to sites of inflammation. Importantly, the site of priming appears to imprint effector T cells with the ability to traffic to particular organs (Agace, 2006). In the gut, CD103+ DCs and stromal cells from Peyer’s patches and mesenteric LNs produce retinoic acid that triggers expression of α4β7 and CCR9 on T cells.
Interactions with their cognate ligands – endothelial-derived MAdCAM and epithelial-derived CCL25 – directs activated T cells to the small intestine. Similarly, T cells primed within the skin-draining inguinal LN preferentially migrate to the skin. This is mediated by cutaneous lymphocyte antigen (CLA), the mouse E/P-selectins, and the chemokine receptors CCR4, CCR8, and CCR10. CCR10 expression is induced by the active form of vitamin D3, locally synthesized by skin DCs (Sigmundsdottir et al., 2007).
TCM cells are defined by the coexpression of LN-homing CD62L and CCR7, and their recirculation through the blood and SLOs. Unlike naive cells, however, they express inflammatory chemokine receptors such as CXCR3 and CXCR4 that may serve as a CCR7-independent LN entry (Scimone, 2004). Recently, the expression of CXCR3 on TCM has been found to have a critical role for their function (Sung et al., 2012). The CD8+ TCM response was directly compared with naive CD8+ T cells after injection of antigen-pulsed DCs or infection with LCMV. Surprisingly, the response to antigenpulsed DCs was similar in naive T and TCM cells except for an enhanced IFN-γ response by the TCM. However, when the same comparisons were made during LCMV infection, TCM had higher CD69 expression, proliferation, and IFN-γ production compared with the naive cells. This was related to the specific recruitment of CXCR3+ TCM into specific T cell zones of the LN with a predominance of LCMV-infected macrophages. CXCR3 ligands chemokines then recruit additional CXCR3+ TCM to the periphery of the LN and sites of active LCMV infection in a feed-forward mechanism that resulted in their quick activation and expansion in response to infection. Thus, CCR7-mediated LN homing coupled with CXCR3 expression on TCM positions these cells to quickly control the spread of virus within the lymphatic system upon rechallenge.
Table of contents :
ABSTRACT
RÉSUMÉ
TABLE OF CONTENTS
LIST OF FIGURES
LIST OF TABLES
REMERCIEMENTS
ABBREVIATIONS
FOREWORD
RESEARCH PLAN
I.! DEVELOP TOOLS FOR SCREENING RARE ANTIGEN-SPECIFIC RESPONSES IN HUMANS
II.! EVALUATE THE IMPACT OF CHRONIC INFECTION ON THE PREIMMUNE REPERTOIRE ….
III.! STUDY THE IMPACT OF CXCR3 RECEPTOR ON INEXPERIENCED T CELLS
CHAPTER 1. GENERAL INTRODUCTION
I.! PREIMMUNE REPERTOIRE
A.! THYMIC DEVELOPMENT
1)! Thymus anatomy and function
2)! Early thymocyte development
3)! Thymic selection of the MHC-restricted preimmune repertoire
4)! Maturation and emigration of mature SP thymocytes
B.! PERIPHERAL NAIVE T CELLS
1)! Recent Thymic Emigrants
2)! Population size and TCR repertoire
3)! Homeostasis and homeostatic proliferation
4)! CD5 expression and dynamic tuning of lymphocytes
5)! Activation, differentiation and activation-induced cell death
6)! Phenotypic and functional diversity
7)! Impact of precursor frequency and diversity
II.! CHRONIC INFLAMMATION
1)! General introduction
2)! HCV as a model of chronic inflammation
(a)! Epidemiology
(b)! Virus genome
(c)! Tropism and entry receptors
(d)! From acute to chronic infection
(e)! Extrahepatic manifestations
(f)! Treatment and clearance benefits
(g)! Antiviral immune responses
3)! HBV as a comparative model of chronic hepatitis
Page 8 / 240 Table of contents
4)! Viro-induced chronic inflammation
5)! T cells and inflammation
III.! T CELL TRAFFICKING
1)! Short introduction about chemokines
2)! Naive T cell trafficking
3)! Effector and resident memory T cells trafficking
4)! Role of CXCR3 in T cell biology
5)! Focus on CXCL10
CHAPTER 2. DEVELOP TOOLS FOR SCREENING RARE ANTIGEN-SPECIFIC RESPONSES
I.! INTRODUCTION
II.! TETRAMER ASSOCIATED MAGNETIC ENRICHMENT (TAME)
A.! PREPARATION OF PMHCI TETRAMERS
B.! PREPARATION OF PHOTOCLEAVABLE PMHCI TETRAMERS
C.! DEVELOPMENT OF TAME FOR HUMAN SAMPLES
D.! TAME INCREASES DETECTION OF AG-SPECIFIC T CELLS BY UP TO 100-FOLD
E.! DETECTION OF NAIVE CD8
T CELLS SPECIFIC FOR HIV GAG P1777-85
F.! ENRICHMENT AND ENUMERATION OF MULTIPLE SPECIFICITIES
III.! DISCUSSION
A.! TAME PERMITS ENUMERATION AND CHARACTERIZATION OF RARE AG-SPECIFIC T CELLS FROM HUMAN PERIPHERAL BLOOD
B.! EPITOPES HAVE CONSERVED PRECURSOR FREQUENCIES AMONG INDIVIDUALS.
IV.! PROSPECTIVES
CHAPTER 3. DEFINE THE INFLUENCE OF CHRONIC HCV INFECTION ON THE PREIMMUNE REPERTOIRE.
I.! INTRODUCTION
II.! EVALUATION OF THE PREIMMUNE REPERTOIRE DURING CHRONIC HCV
A.! GATING STRATEGY
B.! BULK LEVEL
C.! ANTIGEN-SPECIFIC LEVEL
D.! NAIVE T CELL HOMEOSTASIS DURING CHRONIC HCV
III.! DISCUSSION
IV.! PROSPECTIVES
CHAPTER 4. STUDY THE IMPACT OF CXCR3 RECEPTOR ON INEXPERIENCED T CELLS
I.! INTRODUCTION
I.! IN THE THYMUS
II.! IN PERIPHERY
A.! MP CELLS IN THE BLOOD OF NON-IMMUNIZED CXCR3-/- ANIMALS
B.! DISTINCT TCR ACTIVATION PATTERN
C.! MP OTI CELLS IN THE SKIN OF UNIMMUNIZED WT ANIMALS
D.! MP OTI CELLS ARISE IN HOMEOSTATIC ENVIRONMENTS
III.! DISCUSSION
IV.! PROSPECTIVES
CHAPTER 5. GENERAL DISCUSSION
I.! IMMUNOPHENOTYPING CHALLENGES
II.! PREIMMUNE REPERTOIRE AND PERSONALIZED MEDICINE
III.! PREIMMUNE REPERTOIRE AND PERSISTENT VIRUSES
METHODS
I.! GENERATION OF PMHC CLASS I TETRAMERS THROUGH LIGAND EXCHANGE.
II.! TAME PROTOCOL
MANUSCRIPTS
REFERENCES