Get Complete Project Material File(s) Now! »
Myelination process and adaptive myelination
Oligodendrocyte lineage and myelin
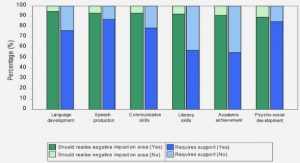
In the CNS, myelin is produced by myelinating oligodendrocytes (OLs) (Rio-Hortega, 1921). Before that, the oligodendrocyte lineage follows a complex differentiation process (Fig.4). Oligodendrocyte progenitor cells (OPCs) are generated during embryogenesis from the ventricular neuroepithelium in the neural tube (Pfeiffer et al., 1993). Then OPCs differentiate in pre-myelinating oligodendrocytes which progress to immature OLs. Finally, these latter mature in myelinating OLs (Levine et al., 1993). Progression through the oligodendrocyte lineage is tightly regulated by a multitude of intrinsic and extrinsic cues, which control myelination both spatially and temporally during development and after myelination. These signals include growth factors, protein kinases, or extracellular matrix molecules (Bauer et al., 2009). Early OPCs are defined by the expression of platelet-derived growth factor receptor α (PDGFrα) and the proteoglycan neural/glial antigen 2 (NG2) (Nishiyama et al., 1996; Pringle et al., 1992). As their differentiation progress, OLs become less proliferative and start to express CNP and GalC (Zalc et al., 1981). Their arborization expand and they finally express myelin proteins (MBP, MAG, PLP) and begin to contact axons (Martini and Schachner, 1986). The maturation to myelinating OLs is achieved when they express the protein MOG (Solly et al., 1996).
In the CNS, in vitro (Watkins et al., 2008) as well as in vivo experiments (Czopka et al., 2013) have demonstrated that myelinating oligodendrocytes establish myelin sheaths in only a few hours. The deposition of the successive myelin layers is led by the inner tongue which wraps around the axon and extends laterally (Fig.5) (Snaidero et al., 2014). The dynamics of the actin cytoskeleton appears finely regulated to trigger myelin wrapping, with an actin polymerization at the leading edge of the inner tongue and subsequent depolymerization (Nawaz et al., 2015; Zuchero et al., 2015).
The morphological (top) and antigenic (bottom) features of OPCs, pre-OLs, mature OLs and myelinating OLs are shown. Adapted from Traiffort et al. 2016.
(A-D) Model of a developing myelin sheath in a wrapped, unwrapped and cross section view. The unwrapped representation shows the geometry and the development of the sheath and the localization of the cytoplasmic channels, which connect the cell body and the growth zone at the inner tongue. The growth zone is colored in pink and compacted myelin in dark violet. The wrapped representation shows the position of the layers when wrapped around the axon. The cross sections show the state of compaction during myelin growth. Adapted from Snaidero et al. 2014 Myelination is a highly regulated process. First, several seminal studies showed that a critical axon diameter is necessary for myelination to occur (Duncan, 1934; Matthews, 1968). Remahl & Hildebrand demonstrated that the spectra of myelinated axon diameter in the corpus callosum vary from 0.2 to 0.7 µm and from 0.6 to 1.2 µm in the spinal cord (Remahl and Hildebrand, 1982). Cultured oligodendrocytes can develop myelin membrane sheets in absence of neurons and can myelinate paraformaldehyde-fixed axons or synthetic fibers (Lee et al., 2012). These results confirmed the role of the axon diameter but also suggested that axonal cues might not be necessary to activate myelination. Moreover, intrinsic properties of OLs play a key role. Using microfibers, Bechler et al. showed that oligodendrocytes respond to fiber diameters and that spinal cord oligodendrocytes generate longer sheaths than cortical oligodendrocytes revealing that oligodendrocytes have regional identity (Bechler et al., 2015). Yet, in vivo, all eligible axons are not myelinated. Thus, several intrinsic axonal cues are known to influence (positively or negatively) myelination (Fig.6) as the axonal ligands Jagged-1 and Delta-1 (Wang et al., 1998), the neurotrophin NGF (Chan et al., 2004), the neuronal cell adhesion molecule PSA-NCAM (Charles et al., 2002a), or the leucine-rich repeat and Ig-domain containing1 (LINGO1) (Mi et al., 2005). The growth factor Nrg-1 and its receptor ErbB have been also implicated in CNS myelination process (Calaora et al., 2001; Canoll et al., 1996).
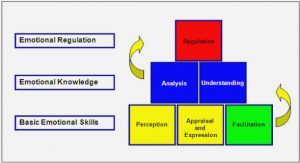
Furthermore, neuronal activity is known to impact myelination (Fig.6). First it was showed that blocking neuronal activity led to reduced OPCs proliferation and myelination (Barres and Raff, 1993; Demerens et al., 1996; Wake et al., 2011). Optogenetic experiments to direct neuronal activity also showed increased OPCs proliferation and survival following neuronal activation, resulting in increased oligodendrogenesis. In these experiments, mature oligodendrocyte number increased along with myelin-basic-protein protein expression and myelin sheath thickness coupled to behavioral improvement (Gibson et al., 2014). Moreover, it has been shown in vitro and in vivo in mice and zebrafish that the choice of the target axons is promoted by neuronal activity (Mitew et al., 2018; Wake et al., 2015). In zebrafish, Mensch et al. have shown that glutamate synaptic vesicular release enhance the number of myelin sheaths made by an individual oligodendrocyte and impact the selection of axons undergoing myelination (Baraban et al., 2018; Hines et al., 2015; Mensch et al., 2015).
Fig.6/ Schematic showing oligodendroglial lineage development and de novo myelination. Action potential firing by active neurons results in the release of neurotransmitters (such as glutamate, GABA, ATP or acetylcholine) and/or growth factors (such as platelet-derived growth factor, brain-derived neurotrophic factor or neuregulin) via synaptic and non-synaptic mechanisms, and exert multifaceted influence upon both oligodendroglial lineage development and axonal ensheathment. Adapted from de Faria Jr et al. 2019.
Recently, the observation of partially myelinated neurons (Tomasi et al., 2012) led to the idea that the myelination pattern along axons and its modulation could participate in regulating axonal conduction and pave the way to the notion of adaptative myelination. Neuronal activity could modulate myelin plasticity which would in turn modulate neuronal networks. In 2014, Tomassy et al. showed that neurons, especially in the superficial layers of the cortex, display distinct longitudinal distribution of myelin suggesting a strategy to modulate long-distance communication (Tomassy et al., 2014). Thus, it has been established that nodes of Ranvier length and interval can modify conduction speed and contribute to the coordination of the coincident arrival of synaptic inputs from multiple axons (Arancibia-Cárcamo et al., 2017; Seidl et al., 2014). Ford et al. showed that internodes length and nodes of Ranvier diameter vary along axonal segments allowing optimization of the conduction velocities to ensure precise timed depolarization (Ford et al., 2015). In mice, OPCs keep proliferating and differentiating in adult CNS, with 5–20% of oligodendrocytes generated during adulthood (Young et al., 2013). Thus, the impact of neuronal activity on myelination in adult brain may result from the ubiquitous presence of OPCs throughout the adult mouse brain (Young et al., 2013). In rodent brain, adult NG2-positive OPCs are constantly migrating through the local environment, retracting, and extending their branched processes (Hughes et al., 2013). Myelin plasticity has been shown to play a role in learning processes. In human, increased brain white matter volume was observed in piano players (Bengtsson et al., 2005) or jugglers (Scholz et al., 2009), also suggesting neuronal activity-induced increased myelin plasticity. Conversely, functional studies showed that socially isolated juvenile mice are hypomyelinated with fewer myelin sheaths produces by OLs. They also exhibit cognitive and behavioral alterations (Makinodan et al., 2012).
Formation of Nodes of Ranvier
Formation of nodes of Ranvier in the CNS is a complex process. Susuki et al. demonstrated that the CNS nodes assembly involves three mechanisms: 1/stabilization of nodal components by ECM ; 2/ paranodal axoglial junctions that function as barriers to restrict the position of nodal proteins; and 3/axonal cytoskeletal scaffolds interacting with nodal markers (Susuki et al., 2013). They show that while mice with a single disrupted mechanism had mostly normal nodes, disruptions of two out of three mechanisms all lead to juvenile lethality, profound motor dysfunction, and significantly reduced Nav channel density. This major result support the hypothesis of complementary and compensatory mechanisms driving myelination (Fig.7).
Fig.7/ Illustration showing the three mechanisms involved in CNS nodes of Ranvier formation ECM, extracellular matrix. Adapted from Susuki et al. Neuron 2013.
Furthermore, the clustering role of oligodendroglial secreted cues was suggested by the Barres laboratory, showing that oligodendroglial secreted factors promote Nav channel clustering in CNS axons in retinal ganglion cell culture, in the absence of axoglial contact (Kaplan et al., 1997). These seminal results were confirmed and extended by our team on hippocampal GABAergic neurons (Freeman et al., 2015) with the identification of the clustering role of a contactin multimolecular complex comprising Phosphacan or Tenascin-R (Dubessy et al., 2019).
Secondly, it has been shown that paranodal junctions are important in the initial clustering of Nav channels (Rasband et al., 1999). In support of a role for paranodal junctions in the assembly of CNS nodes, researchers reconstituted paranodes by transgenic expression of glial NF-155 on a NF-null background. They found that this rescued the correct assembly of CNS nodes of Ranvier in the absence of NF186. However, data from paranodal mutant mice also suggested that paranodal junctions are dispensable for node assembly. Indeed, Nav channels accumulate at nodes in NF-null mice rescued with transgenic NF-186 (no reconstitution of the paranodal junctions) (Zonta et al., 2008).
Thirdly, concerning the role of cytoskeletal scaffolds, the interactions between AnkyrinG and CAMs or ion channels may promote their stable and restricted localization at nodes. AnkyrinG recruits βIV-spectrin to nodes, which in turn provides further linkage to the axonal cytoskeleton (Yang et al., 2007). Thus, the βIV-spectrin and ankyrinG based axonal cytoskeleton are important for stabilization of nodal Nav channel complexes. Furthermore, the work of Barry et al. revealed that AnkyrinG functions as an adaptor that links Nav channels to the anterograde molecular motor KIF5B during axonal transport suggesting that the axonal localization of Nav channels could rely on its interaction with AnkyrinG (Barry et al., 2014). More recently, our team showed that some nodal proteins are partially co-transported along the axon, suggesting a partial pre-assembly of the nodal complex prior to membrane targeting (Thetiot et al., 2020). Moreover, Nav channel binding to ankyrinG is both necessary and sufficient for channel clustering (Gasser et al., 2012). However, mice lacking nodal βIV-spectrin, which links AnkyrinG and Nav channels to the actin cytoskeleton, have relatively normal CNS nodes (Komada and Soriano, 2002). Indeed, compensatory mechanisms are involved: β1 spectrin, together with AnkyrinR (AnkR), could compensate for the loss of nodal AnkG and βIV spectrin (Ho et al., 2014; Liu et al., 2020).
Interestingly, nodal clustering mechanism may differ between neuronal subpopulations. Indeed, our team demonstrated the existence of nodal Nav clusters preceding myelination in hippocampus experimental models in vitro and in vivo on GABAergic neurons, but not on pyramidal cells, suggesting that different mechanisms are at play to form nodes of Ranvier in the CNS. These node-like clusters correlated with accelerated axonal conduction, as shown by single neuron electrophysiological recording (Freeman et al., 2015) and might also play a key role in initiating myelination (Thetiot et al., 2020).
Demyelination and remyelination processes in Multiple Sclerosis and its experimental models
Natural course of Multiple Sclerosis
Multiple sclerosis (MS) is a chronic inflammatory demyelinating and neurodegenerative disease of the CNS leading to multiple foci of demyelination in white and grey matter of the brain and spinal cord. It is an autoimmune disease with predisposing genetic and environmental factors (Reich et al., 2018).
It is the most prevalent chronic inflammatory disease of the CNS, affecting >2 million people worldwide and currently incurable (GBD 2015 Neurological Disorders Collaborator Group, 2017). In Europe, prevalence is 1 out of 1000 people and thus is a frequent disease which constitute the first cause of non-traumatic handicap in young adults (Dubessy et al., 2014).
Some risk factors have been identified but remained scarce despite extensive clinical research. Smoking, and geographical gradient (at the expense of cold latitudes) are the two main known risk factors. Obesity, and mononucleosis are also associated with enhanced risk for developing MS. There is a sex ratio of 3 women for a man and the median age of onset is 30 (Compston and Coles, 2002; Reich et al., 2018).
The natural course of the disease is characterized in 85% of patients by the succession of relapses (relapsing-remitting phase) with various functional impairments (Fig.8): motor or sensory deficits, balance, or gait impairment. Oculomotor, optical, or urinary deficiencies are also common. For the 15% remaining patients, evolution is out of hand progressive (primary progressive) and linked to neurodegenerative processes. Among relapsing-remitting patients, around 50% will develop a secondary progressive form after 15-20 years of disease evolution (Dubessy et al., 2014).
To date, the main therapeutic angle used in MS is immunosuppressive/immunomodulatory therapy preventing inflammation and demyelination and thus relapses (Cree et al., 2019). On the other hand, the neurodegenerative part of the disease lacks therapeutical strategies. To achieve efficient immunosuppression in MS, some drugs decrease activation or proliferation of lymphocytes (teriflunomide, dimethyl-fumarate, interferonβ, glatiramer acetate), others prevent lymphocytes circulation (fingolimod) or their entry in the brain (natalizumab). Lastly, ocrelizumab suppresses a sub population of B lymphocytes (Rommer et al., 2019), probably interfering with antigen cell presentation.
Demyelination in MS
The demyelinated white matter lesions, responsible for relapses in MS, are characterized by inflammatory infiltrates composed of T cells, B cells and macrophages/microglia, demyelination, axonal loss, varying degrees of remyelination and glial scar formation. But white matter lesions from relapsing-remitting and chronic progressive disease significantly differ from each other.
The main white matter lesion type in relapsing multiple sclerosis is the actively demyelinating, inflammatory lesion, representing 35% of all lesions (Frischer et al., 2015). Active lesions are characterized by areas with sharp limits of demyelination. They can be either demyelinating or post-demyelinating according to macrophages population and their cytoplasm content (myelin degradation products). If demyelinating, myelin degradation products are visible in macrophages cytoplasm. Four histopathological profiles with active lesions have been described in MS (Lucchinetti et al., 2000) (Fig.9):
Pattern I is characterized by T-lymphocytes and macrophages inflammation.
Pattern II is very similar to pattern I, adding the presence of IgG and complement C9 deposition.
Pattern III showed T-lymphocytes and macrophages inflammation, no IgG deposits, ill-defined lesions, and oligodendrocytes apoptosis.
Pattern IV is similar to pattern III and showed T-lymphocytes and macrophages inflammation, no IgG deposits, loss of oligodendrocytes without apoptosis.
Pattern II showing lesions with sharp limits (a; b), massive C9 deposition at the actively demyelinating border (e).
Pattern III showing lesions with ill-defined borders (c, d), apoptotic oligodendrocytes (g-k). Pattern IV showing DNA fragmentation of oligodendrocytes is seen in the periplaque white matter (o).
Very interestingly, at a given time point of the disease—as reflected in autopsy cases—the patterns of demyelination were heterogeneous between patients but were homogenous within multiple active lesions from the same patient. This suggests that various lesion mechanisms might exist according to each patient. White matter lesions of patients suffering from progressive multiple sclerosis are different and have originally been described as slowly expanding lesions. They are considered to be the morphological correlate of disease progression and are characterized by an accumulation of macrophages at the lesion edge that mediate active ongoing myelin breakdown and axonal damage (Prineas et al., 2001). However, a recent classification characterized more precisely these lesions calling them mixed active/inactive lesions (Fig.10) (Kuhlmann et al., 2017).
Thus, mixed active/inactive lesions are characterized by areas with sharp limits of demyelination and a rim of macrophages at the lesion edge. Two types are described, again depending on macrophages activity:
– Demyelinating (former smoldering or slowly expanding lesions)
– Post demyelinating (former chronic active lesions)
The significance of these mixed active/inactive lesions is still under debate (Jäckle et al., 2020). They are classically associated with the progressive stages of the disease. By applying the microglia-specific marker TMEM119, researchers demonstrate that cells accumulating at the lesion edge almost exclusively belonged to the microglial lineage (and were not monocyte-derived macrophages). By using a panel of markers characterizing their phenotype, they observed a preferential accumulation of pro-inflammatory cells at the lesion edge, indicating a crucial role of these cells in lesion progression. MRI studies identified a persistent phase rim (Absinta et al., 2016) or an iron rim at the lesion edge (Dal-Bianco et al., 2017) as potential in vivo markers for neuroimaging. These lesions may therefore be useful as a prognostic tool in multiple sclerosis patients (Luchetti et al., 2018).
Lastly, inactive lesions are fully demyelinated but without macrophages presence and characterized by a glial scar in their center with accumulation of astrocytes.
An extensive analysis of white matter plaques in a large sample of MS autopsies showed that active plaques were most often found in early disease, whereas at later stages, mixed active/inactive and inactive lesions predominated. The presence of early active plaques rapidly declined with disease duration. Moreover, depending on the clinical course (relapsing-remitting vs. progressive MS), plaque type distribution differed significantly: most plaques in acute monophasic and relapsing-remitting MS (RRMS) were active. Disease duration, clinical course, age, and gender contribute to the dynamic nature of white matter MS pathology (Frischer et al., 2015).
Furthermore, pathological processes without demyelination have also been described in MS supporting the idea that MS is not only a myelin disease. Focal axonal degeneration before demyelination (Nikić et al., 2011) and acute axonal injury without any demyelination after experimental oligodendrocytes ablation were found (Oluich et al., 2012) in MS experimental models and MS tissues. Howell et al. showed that a significant early alteration in Nfasc155+ paranodal structures occurs within and adjacent to actively demyelinating white matter MS lesions that are associated with altered axonal organization (Howell et al., 2006). Moreover, focal changes have been documented in normal-appearing white matter of MS months to years before the appearance of MRI gadolinium-enhancing lesions. In these foci, clusters of activated microglia are found in the absence of demyelination or clear leukocyte infiltration, distinguishing them from the traditional demyelinating active and mixed active/inactive lesions (van der Valk and Amor, 2009).
c) Remyelination
i. Remyelination in experimental models
Richard and Mary Bunge demonstrated after demyelination induced in subpial cord by cerebrospinal fluid exchange that demyelinated axons can acquire new myelin sheaths (Bunge et al., 1961). Remyelination relies on the rapid repopulation of the demyelinated lesion with glial progenitor cells and their subsequent differentiation into myelinating oligodendrocytes. Thanks to this physiological process an efficient conduction is restored (Smith et al., 1979). Studies of experimental models of demyelination, induced either by immunological, viral, or chemical means, have demonstrated that remyelination is usually very rapid and efficient and is associated with improved neurological function (Franklin and Goldman, 2015).
Indeed, long ago it was shown that the degree of axonal loss in experimental allergic encephalomyelitis (EAE) is greater in areas of active demyelination than in areas with remyelination (Kornek et al., 2000). Pohl et al. reported that a selective genetic ablation of OLs to induce demyelination was followed by axonal injury (Pohl et al., 2011). Several more recent studies demonstrated that remyelination favors neuroprotection. First, Irvine & Blakemore showed that rescuing remyelination in irradiated mice (to prevent endogenous remyelination) after cuprizone induced demyelination allows to decrease axonal loss (Irvine and Blakemore, 2008). Moreover, Mei et al. showed that accelerated remyelination during inflammatory demyelination prevents axonal loss and improves functional recovery (Mei et al., 2016).
Remyelination follows several crucial steps which have been extensively studied in this last decade (Fig.11). The first question was to isolate the cell population leading to the generation of myelinating OLs. Tripathi et al. examined the fates of PDGFRα/NG2 cells in the mouse spinal cord during experimental autoimmune encephalomyelitis showing that most of these cells differentiate in OLs expressing myelin markers as CNP or Opalin. These results suggest that adult OPCs are the major source of new OLs during remyelination (Gensert and Goldman, 1997; Levine and Reynolds, 1999; Tripathi et al., 2010). On the other hand, several studies have shown that human mature oligodendrocytes transplanted into demyelinated areas of the rat spinal cord survived but were unable to remyelinate (Crawford et al., 2016; Keirstead and Blakemore, 1997; Targett et al., 1996). But, interestingly, others suggested that new myelin sheaths can be generated by existing oligodendrocytes without the need for de novo oligodendrogliogenesis (Duncan et al., 2018; Wood and Bunge, 1991).
Fig.11/ The biology of remyelination. Following damage to myelinated areas in the CNS, remyelination is initiated by activation of oligodendrocyte progenitor cells (OPCs). These become activated (as represented by the color change), divide, and form new oligodendrocytes. Note the presence of macrophages in the lesion. Following oligodendrocyte differentiation, myelin formation proceeds in three steps, as shown in the sequence illustrated in the lower panel: the formation of multiple processes and the expression of myelin proteins such as myelin basic protein, the initial wrapping of the axon by an elaboration of myelin membrane and, finally, the formation of multilayered and compacted sheaths by the continued elaboration of membrane, further wrapping of the axon and extrusion of the cytoplasm. Adapted from Franklin & French-Constant 2017.
For remyelination to occur, activation (visible by morphological and behavioral changes), proliferation, and migration of OPCs are necessary. The order in which these events occur is still under debate. Some transcription factors (TCF7L2 and SOX2), normally absent in the normal CNS OLs lineage, are detected after myelin injury, permitting enhanced proliferation, and priming for differentiation (Fancy et al., 2009). Next, the importance of migration was underlined by Boyd et al. who showed that some MS lesions lack sufficient OPCs to drive remyelination suggesting a failure in migration (Boyd et al., 2013). Moreover, it was demonstrated in the lab that increasing OPCs recruitment towards demyelinated areas by overexpression of attractive guidance cues (Semaphorin 3F) accelerates remyelination after experimental demyelination (Piaton et al., 2011).
Thirdly, to myelinate denuded axons, OPCs need to differentiate in myelinating OLs. To do so, OPCs must exit the cell cycle (Casaccia-Bonnefil et al., 1997). How OPCs switch from a proliferating to a differentiating stage remains elusive. One hypothesis is based on cell density. When the number of OPCs reaches a certain level, proliferation stops, and differentiation starts (Hughes et al., 2013). Others investigated about potential positive or negative cues. Several studies showed that myelin debris could inhibit OPCs differentiation (Plemel et al., 2013; Robinson and Miller, 1999). Using inhibitors of the retinoid X receptor pathway, it was showed that aging macrophages are less effective to clear myelin debris, leading to inhibition of OPCs differentiation (Natrajan et al., 2015). Glial environment can also promote OPCs differentiation. Thus, it has been shown that activated microglia can secret various cues promoting remyelination (Miron and Franklin, 2014; Psachoulia et al., 2016).
Furthermore, it is now clear from an abundant literature on the subject that other glial cells contribute to this process of myelin repair. A pro-remyelinating environment including cytokines, growth factors, ECM, and adhesion molecules, expressed in an appropriate manner, participates to favor activation, proliferation, migration, and differentiation of OPCs (Franklin, 2002). In this context, Miron et al. (Miron et al., 2013) showed that macrophage switch to M2 phenotype drives OPCs differentiation. Preventing this switch could thus prevent efficient repair. Moreover, El Behi et al. showed, comparing remyelination after grafting lymphocytes from healthy donors or from MS patients in spinal cord demyelinated lesions that lymphocytes derived cytokines help OPCs differentiation through microglia modulation (El Behi et al., 2017). Others showed the role of neuronal activity on repair. Electrically active demyelinated axons can form new glutamatergic synapses with OPCs present within areas of demyelination. Through sensing axonal activity via AMPA and kainate receptors, OPCs can exit the cell cycle and undergo differentiation (Etxeberria et al., 2010; Gautier et al., 2015). More recently, Ortiz et al. using optogenetic experiments reported an increase of OPC differentiation and extensive remyelination after activation of demyelinated axons (Ortiz et al., 2019).
Regarding astrocytes, there are also evidence that they can help to clear debris (Skripuletz et al., 2013). They are abundant in glial scar in inactive lesions. Whether it brings more damage or inhibits repair is still under debate (Pekny et al., 2014). For example, it has been suggested that reactive astrocytosis is also common in the normal appearing white matter (NAWM) (Zeis et al., 2008). On the other hand, studies using ethidium bromide demyelination confirmed the need for these cells in remyelination, as elimination of astrocytes resulted in remyelination only by Schwann cells, unless transplanted astrocytes were reintroduced (Franklin et al., 1991). Furthermore, it has been showed that perinodal astrocytes can regulate myelin structure (thickness and gap length) and could thus contribute to adaptative (re)myelination (Dutta et al., 2018).
Remyelination in MS
After the demyelinating insult, endogenous remyelination can also occur spontaneously in MS (Prineas and Connell, 1979). Classically, remyelinated areas are known in MS as “shadow plaques”. Shadow plaques are fully remyelinated lesions in MS brains (Fig.12). They are called “shadow” because of the pale staining compared to normally myelinated areas. It is related to the thinner myelin sheaths and shorter myelin internodes typical of newly formed myelin in remyelinated areas. Thus, shadow plaques demonstrate that complete repair of MS plaques is possible, although it is more common to observe only limited repair at the edge of lesions. Furthermore, the location of a lesion influences the likelihood of remyelination, with subcortical lesions showing more signs of remyelination than periventricular or cerebellar lesions (Goldschmidt et al., 2009).
The section is stained with Luxol Fast Blue to reveal myelinated areas in the subcortical white matter. The green arrows indicate three areas from which the myelin staining is absent, representing three foci or plaques of chronic demyelination. The red arrows indicate ‘shadow plaques’, in which the demyelinated axons have undergone remyelination. Adapted from Franklin 2002.
Even if we know that this process is partial and becomes rarer with age and disease duration, it has been suggested that remyelination in MS may be more extensive than previously thought. One detailed neuropathological study of two MS cases showed that nearly 50% of white matter analyzed was remyelinated (or remyelinating). Increased density of macrophages and microglia at the lesion border correlated significantly with more extensive remyelination. (Patani et al., 2007). In another study, in 20% of the patients, the extent of remyelination was extensive with 60–96% of the global lesion area remyelinated (Patrikios et al., 2006). Subgroups of MS patients with either extensive or limited remyelination were identified, suggesting that in addition, genetic factors may influence the ability of lesions to remyelinate. Moreover, it has been suggested that remyelinated areas could be difficult to distinguish from intact white matter (Neumann et al., 2020) implying that remyelination might be underestimated in MS brains. Moreover, a PET-MRI study using a myelin marker ([11C]PIB) showed a great variability of myelin content changes between patients, that might indicate inter-individual myelination capacity. This PET study also demonstrated that dynamic remyelination was inversely correlated with clinical disability (Bodini et al., 2016). El behi et al., using the lymphocytes graft paradigm described above, confirmed diverse remyelination patterns depending on these different patients (El Behi et al., 2017).
Table of contents :
INTRODUCTION
I. Myelin, nodes of Ranvier and the myelination process
a) Composition and organization of myelinated fibers
b) Functional properties of myelin and nodes of Ranvier
c) Myelination process and adaptive myelination
i. Oligodendrocyte lineage and myelin
ii. Formation of Nodes of Ranvier
II. Demyelination and remyelination processes in Multiple Sclerosis and its experimental models
a) Natural course of Multiple Sclerosis
b) Demyelination in MS
c) Remyelination
i. Remyelination in experimental models
ii. Remyelination in MS
d) Nodes of Ranvier in demyelination and remyelination
i. Nodes of Ranvier fate during demyelination
ii. Nodes of Ranvier assembly in remyelination
iii. Consequence of Nodes of Ranvier alterations on neuronal physiology
iv. Nodes of Ranvier and glial cells (Fig.16)
III. Microglia: a new major player in MS
a) Description and function of microglial cells
b) Classification of microglia phenotypes in health and disease
c) A dynamic and social cell
d) Microglia and Multiple Sclerosis: a dual role.
i. A role in inflammation
ii. Microglial role in repair
GENERAL DISCUSSION
I. Characteristics of node-microglia interaction in control tissue
II. Characteristics of node-microglia interaction in pathological states
III. Node-microglia interaction could participate in the microglial switch in repair
IV. Microglial profiles observed in human tissues
V. Nodes of Ranvier as a glial-communication hub
CONCLUSION