Get Complete Project Material File(s) Now! »
Associated anxiolytics: the benzodiazepines family
Chemistry
The discovery of benzodiazepines (BZDs) is an example of serendipity. It is the result of the work of Leo Sternbach, an Austro-Hungarian pharmacologist, who worked on quinolone/quinazoline derivatives for the manufacture of dyes. After his immigration during World War II to the United States, he started to work for Hoffman La Roche, where he had to find a molecule to replace meprobamate, the current anti-anxiety drug (cf. 3.3.2). Forced to stop his research, he put several of his samples aside. It was a few years later, with the work of a colleague that strong calming properties were associated to one of the quinolone derivatives, combined with a low toxicity in vivo. Chlordiazepoxide (FIGURE 2.8) was thus discovered (and sold in 1960), followed some years later by diazepam (FIGURE 2.8, marketed in 1963) and both would revolutionise the anti-anxiety drugs market.
Chemically, these two molecules are derived from the same structure, the benzodiazepine ring that is the combination of a benzene and a diazepine ring. The diazepine is a heterocycle with two nitrogen and five carbon atoms and the maximum possible number of double bonds. Nitrogen atoms can be present in positions 1,4, 1,5 or 2,3 (FIGURE 2.7). Three classes of BZDs can then be discerned, but most prescribed benzodiazepines are the 1,4 due to their more interesting pharmacological properties (FIGURE 2.8).
Substitutions in the first position increase activity via an alkylation.
Substitutes in the second position with an electronegative atom (O or N) were more common in the first generation of BZDs whereas more recent BZDs have fewer substitutions in this position.
If there is no substitution in the third position, or if it is a hydroxyl functional group (OH, e.g. oxazepam), the polarity of the molecule is increased; a glucuronosylation in this position allows a faster elimination.
Eventually, substitutions on the benzene ring may also take place: an ortho-substitution with a fluorine or a chlorine atom increase the activity of the molecule (electron-withdrawing group); another ring like a cyclohexenil ring can even substitute the benzene ring (e.g. in tetrazepam, a muscle relaxant BZD) or a pyridyl ring (e.g. in bromazepam).
The BZDs have basic properties, which allow them to bind to plasma proteins, favouring a fast blood transport. They are also very lipophilic, which allow them to cross the blood brain barrier, a common obstacle to the development of psychoactive drugs.
Some benzodiazepines-like molecules were also found in both cow and human milk (Medina et al, 1988; Peña et al, 1991). No further attempt to identify their origin and nature was yet made.
Chlordiazepoxide: first BZD to be discovered (1960). Diazepam: second BZD to be discovered (1963); often used as the reference BZD in animal studies. Alprazolam: most sold BZD in France. Clobazam: an example of a 1,5 BZD. Oxazepam: an example of hydroxylation in the third position. Flunitrazepam: an example of NO2 substitution in the seventh position (hypnotic BZD). Tetrazepam: an example of benzene ring substitution (muscle relaxant BZD). Bromazepam: an example of benzene ring substitution with a brome in seventh position.
Therapeutic effects
BZDs are psychoactive drugs and belong to the depressants family, which decrease the CNS activity and hence exert sedative effects. BZDs are then mostly prescribed for their anxiolytic, hypnotic, anticonvulsant and muscle relaxant properties, while they also exhibit amnestic effects.
Different forms of administration can be used. Oral administration ensures a quick action with an effect obtained a few hours after ingestion (TABLE 2.4). Effects are slower than oral administration via an intramuscular injection. Eventually, a rectal administration is used only when an intravenous injection cannot be performed: it is however optimal for a fast action in the CNS.
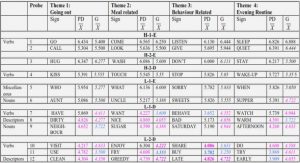
In 2013, twenty-two BZDs were commercialised in France and a few therapeutic effects are favoured depending on the molecule structure and half-life. The majority of them is prescribed for their anxiolytic and/or hypnotic properties (TABLE 2.3 and TABLE 2.4) (ANSM, 2013). It is however sometimes hard to distinguish the two effects: indeed anxiolytic BZDs also triggers drowsiness while hypnotic BZDs are also known to be minor tranquilisers. Anxiolytic BZDs are prescribed to deal with the different anxiety-disorders described later (cf. 3.3.1) (Ashton, 1994).
Diazepam is on the World Health Organization’s List of Essential Medicines, the most important medication needed in a basic health system, for both its anxiolytic and anticonvulsant properties (World Health Organization, 2015). Lorazepam and midazolam are also on the list for their anticonvulsant and sedative effects, respectively.
Benzodiazepines anxiolytic effects were also unearthed in several animals’ models due to the predictive criteria which was used to develop these tests (cf. 4.1.1), e.g. elevated plus-maze (Handley and Mithani, 1984), light-dark box (Crawley, 1981), open-field (Prut and Belzung, 2003) or conditioned defensive burying (Treit et al, 1981).
Mechanism of action
The receptors for BZDs are exclusively located in the CNS at the synaptic level and their pharmacological efficiency is dependent on the affinity of BZDs for these receptors (Möhler and Okada, 1977). Later, these receptors for BZDs have been shown to co-localise with the GABAA receptors, before the identification of a specific site directly on the GABAA receptor (Schoch et al, 1985; Sieghart and Sperk, 2002). The BZDs act as allosteric modulators of the GABAA receptor. The BZDs link to a site different from the GABA site and then enhance the affinity of GABA and increase the probability of the chloride channel to open, resulting in an increase influx of chloride ions and thus an hyperpolarisation of the neuron (TABLE 2.5) (Costa and Guidotti, 1979; Millan, 2003). The facts that GABA is needed for BZDs to exert their effect may explain the lesser toxicity of these drugs compared to other GABAA receptor ligands such as ethanol or barbiturates which directly act with the chloride channel (Gray, 1982).
Table of contents :
Part I – General introduction
1 Bioactive peptides from milk proteins
2 GABAergic system and α-casozepine
3 Behavioural and neural bases of anxiety
4 Rodents’ models of anxiety
Part II – Personal work
1 Objectives of the research project
2 Evaluation of the mices based on their basal levels of anxiety
3 Modulation of neural activity in mice induced by α-casozepine
4 Evaluation of the anxiolytic activity of, and the modulation of brain activity by YLGYL, a derivative from α-casozepine
5 Investigations concerning the mediation of anxiolytic-like properties of α-casozepine
Part III – General discussion and conclusion
1 Deciphering the central mode of action of α-casozepine
2 Conclusion and Persectives
Part IV – Annex
1 Résumé substantiel
2 List of communications