Get Complete Project Material File(s) Now! »
Identification of the outcomes in relation to ADEs
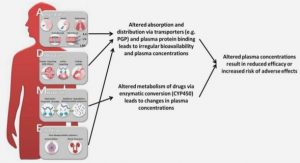
The present section describes how the list of traced outcomes is defined. The ADE can be defined as injuries due to medication management rather than the underlying condition of the patient [IOM 2007]. Those injuries may consist of clinical or paraclinical signis that result from a drug intake, a dose modification, or a drug discontinuation. Those conditions are commonly described as the use of a drug [Gurwitz 2000]. All the ADEs that have been observed for a given drug are described in the related SPC (Summary of Product Characteristics). It is reasonable to think that the union of all the SPCs provides a list of all the potential outcomes related to drugs, according to the current knowledge.
In order to prepare data-mining-based rule induction, a list of outcomes is necessary. The drugs that are known to lead to those outcomes are not considered: only the list of the outcomes is used. The main source consists of the knowledge from SPCs validated by the AFSSAPS, the French national drug administration. The knowledge is collected by the Vidal Company and maintained in their knowledge database under the form of rules. From those rules, 228 different kinds of outcomes are precisely described. Those outcomes are clinical and paraclinical signs of ADEs. All of those 228 outcomes are examined in order to find if and how they can be traced in the EHRs.
Description of Outcomes from the SPCs
The outcomes from the SPCs described in the Vidal database belong to two major categories:
SPC clinical outcomes:
– Definition: these outcomes are observed only by means of clinical examination of the patient.
– Example: the onset of urticarial reaction following the introduction of a drug during the hospitalization.
– Number: 149 different clinical outcomes are described in the SPCs Automated detection of Adverse Drug Events by Data Mining of Electronic Health Records Emmanuel Chazard, PhD Thesis Page 69 of 262 SPC laboratory-related outcomes:
– Definition: these outcomes can be objectified by measuring a laboratory parameter.
– Example: the occurrence of an acute renal failure during the stay.
– Number: 79 different paraclinical outcomes are described in the SPCs A significant number of outcomes have clinical and paraclinical definitions; every outcome is nevertheless assigned to a single category in the previous description. The list of the outcomes is presented hereafter. As many outcomes are very similar to one another, they are grouped into the same label and the initial number of different outcomes is displayed in brackets (Figure 17).
Tracing of SPC Outcomes in this work
The appearance of the outcomes listed above has to be traced in the data. This is possible through different ways with respect to the category defined before. SPC clinical outcomes:
– Properties: o Most of them can be defined by means of ICD10 codes. o Some of them can indirectly be traced by means of laboratory results.
For instance, a hemorrhage under Vitamin K Antagonists is strongly linked to an increase of the INR, and might be followed by a decrease of the Hemoglobin blood level. o Some of them can be traced as drug administrations. For instance, a hemorrhage under VKA is often followed by a Vitamin K administration.
– Implementation: o ICD10-related outcomes cannot be used as is. Indeed, the diagnoses are encoded retrospectively at the discharge of the patient, and the ICD10 codes are provided without any date. As a consequence, it is not possible to know if a diagnosis such as “hemorrhage” is the reason of admission or a side effect that occurred during the hospitalization.
Most of the time, it is the reason of admission.
o As much as possible, clinical outcomes are translated into laboratoryrelated signals or into drug-prescription-related signals. SPC laboratory-related outcomes:
– Properties: these outcomes can be objectified by a deviation in laboratory results.
– Implementation: all the paraclinical outcomes that are traceable in the laboratory results of the dataset are taken into account. Some of these outcomes are traced by means of combinations of several parameters, e.g. pancytopenia is the combination of anemia, leucopenia and thrombopenia.
The use of outcomes that are traced through abnormalities in lab results (e.g. hyperkalemia) or specific drug prescriptions (e.g. specific antidote) presents multiple advantages:
– The values are measured several times and the detailed chronology is available.
Evaluation of the clinical impact of ADEs
Adverse Drug Events cannot consist only of biological abnormalities because the definition describes effects which [are] noxious to the patients [EC 2001]. For that reason, it is necessary to find some ways to assess the clinical impact of the ADE we might be able to detect, such as death, higher length of stay, change in medication management, etc.
The main idea is that some variables could help to automatically assess the clinical impact of adverse drug events. In order to identify such variables, 90 hospitalizations with adverse events are reviewed by physicians assisted by a computer scientist. The experts are asked to review carefully the stays and to describe in what ways the various observed outcomes could have consequences on the patient or on his stay, such as “death”, or “longer hospitalization”.
The physicians are asked to answer the following questions:
– How did you notice the consequences of the adverse event?
– Is it possible to generalize those criteria? Would new aggregated variables be useful for that?
As an example, three clinical cases of ADEs, and the corresponding variables are presented in Table 14, Table 15 & Table 16. The result of this procedure is followed up and generalized on every available variable.
Table of contents :
1. INTRODUCTION
1.1. DEFINITION OF ADVERSE DRUG EVENTS
1.2. STATE OF THE ART IN ADVERSE DRUG EVENTS DETECTION
1.3. STATE OF THE ART IN DATA MINING
1.3.1. Introduction
1.3.2. Requirements of data mining
1.3.3. Review of the methods
1.3.4. Conclusion of the State of the Art in Data Mining
1.4. THE PSIP PROJECT
1.4.1. Project summary
1.4.2. Project objectives
1.4.3. Structure of the project
1.5. OBJECTIVES OF THE PRESENT WORK
1.6. ARIANE’S THREAD
2. MATERIAL
2.1. OVERVIEW
2.2. DEFINITION OF A COMMON DATA MODEL
2.2.1. Consideration about normalization
2.2.2. Available data
2.2.3. Terminologies
2.2.4. Description of the data model
2.2.5. Iterative quality control
2.3. DATA EXTRACTION
2.4. EXTRACTION OF THE DRUG CODES FROM THE FREE-TEXT REPORTS
2.4.1. Objectives
2.4.2. The F-MTI tool
2.4.3. Main use of Semantic Mining in the present work
2.5. ADE DETECTION RULES EXTRACTED FROM THE SPCS
2.5.1. General content
2.5.2. Format of the rules
2.5.3. Usability of the rules
3. METHOD
3.1. INTRODUCTION
3.2. IDENTIFICATION OF THE OUTCOMES IN RELATION TO ADES
3.2.1. Principle
3.2.2. Description of Outcomes from the SPCs
Automated detection of Adverse Drug Events by Data Mining of Electronic Health Records
Emmanuel Chazard, PhD Thesis Page 8 of 262
3.2.3. Tracing of SPC Outcomes in this work
3.3. EVALUATION OF THE CLINICAL IMPACT OF ADES
3.4. DATA MINING: A FIVE-STEP PROCEDURE
3.4.1. Step 1: Transformation of the data into event (data aggregation)
3.4.2. Step 2: qualification of the events as “potential condition” or “potential outcome”
3.4.3. Step 3: statistical associations between potential conditions and outcomes
3.4.4. Step 4: filtering of the associations
3.4.5. Step 5: validation of the rules
3.5. CENTRAL RULE REPOSITORY
3.5.1. Knowledge integrated in the Central rule repository
3.5.2. Rule description and storage in the central rule repository
3.6. CONCLUSION
4. RESULTS
4.1. OVERVIEW OF THE CHAPTER
4.2. OVERVIEW OF DATA-MINING RESULTS
4.3. DECISION RULES INTEGRATED IN THE CENTRAL RULE REPOSITORY
4.3.1. Validated rules
4.3.2. Detailed example of five rules
4.3.3. Classification / Overview of the rules
4.4. EVALUATION OF THE ADE DETECTION: PRELIMINARY RESULTS
4.4.1. Cases of Hyperkalemia (K+>5.3 mmol/l)
4.4.2. Cases of VKA overdose (INR>4.9)
4.4.3. All kinds of potential ADE
4.5. PRESENTATION OF THE RESULTS: THE EXPERT EXPLORER AND THE SCORECARDS
4.5.1. Description of the Expert Explorer
4.5.2. Description of the Scorecards
4.5.3. Use case example of the web tools for ADE discovery in databases
5. DISCUSSION
5.1. CONTRIBUTION OF THE PRESENT WORK TO ADE DETECTION
5.2. DISCUSSION OF THE METHOD
5.3. PERSPECTIVES
5.3.1. Reusability of the tools
5.3.2. Meta-rules for the implementation into a CDSS
5.3.3. Reusability of the rules described using XML files
6. CONCLUSION
7. REFERENCES
Automated detection of Adverse Drug Events by Data Mining of Electronic Health Records
Emmanuel Chazard, PhD Thesis Page 9 of 262
8. ARTICLES
8.1. PUBMED REFERENCES
8.2. SCIENCE DIRECT REFERENCES
9. APPENDIX 1: TIME REQUIRED TO PERFORM THE DATA MINING TASK
9.1. OBJECTIVE OF THIS CHAPTER
9.2. DESCRIPTION OF THE TASKS AND NEEDED TIME
9.2.1. Getting data from a hospital, first time
9.2.2. Getting data from a hospital, next times
9.2.3. Aggregating the data
9.2.4. Discovering new rules
9.2.5. Testing the rules of the central repository on an aggregated dataset
9.2.6. Publishing the datasets and the rules occurrences on the web tools
9.3. “HOW MUCH TIME…”: USE CASE POINT OF VIEW
9.3.1. Already known partner: computing statistics
9.3.2. New partner: computing statistics
9.3.3. Discovering some new rules
10. APPENDIX 2: ODP DESCRIPTION OF THE EXPERT EXPLORER
10.1. USER REQUIREMENT AND ENTERPRISE VIEWPOINT
10.1.1. Use case 1
10.1.2. Use case 2
10.1.3. Use case 3
10.2. INFORMATION VIEWPOINT
10.3. COMPUTATIONAL VIEWPOINT
10.4. ENGINEERING VIEWPOINT
10.5. TECHNOLOGY VIEWPOINT
10.6. DETAILED DESCRIPTION OF THE INTERFACE AND USE FLOW
10.6.1. Introduction
10.6.2. Implementation and availability
10.6.3. First Page
10.6.4. Data sets
10.6.5. Reports
10.6.6. Rules
10.6.7. Visualization of a stay
10.6.8. User accounts
10.6.9. Experts’ queries validation task
10.6.10. Administration
11. APPENDIX 3: ODP DESCRIPTION OF THE SCORECARDS
11.1. USER REQUIREMENTS AND ENTERPRISE POINT OF VIEW
Automated detection of Adverse Drug Events by Data Mining of Electronic Health Records
Emmanuel Chazard, PhD Thesis Page 10 of 262
11.1.1. Use case
11.2. INFORMATION VIEW POINT
11.3. COMPUTATIONAL VIEWPOINT
11.4. ENGINEERING VIEWPOINT
11.5. TECHNOLOGY VIEWPOINT
11.6. DETAILED DESCRIPTION OF THE INTERFACE AND USE FLOW
11.6.1. Introduction
11.6.2. Interface design and development
11.6.3. First page of the Scorecards
11.6.4. “Synthesis and Edition of detailed statistics” Page
11.6.5. “Detailed statistics” Page
11.6.6. “Review cases” Page
11.6.7. “Review cases” questionnaire
12. APPENDIX 4: DESCRIPTION OF THE OUTPUT OF THIS WORK (USE OF THE XML FILES)
12.1.MAPPING XML FILES
12.1.1. Overview
12.1.2. Diagnosis mapping: mapping_diag.xml
12.1.3. Drugs mapping: mapping_drug.xml
12.1.4. Lab results mapping: mapping_lab.xml
12.2. RULES XML FILES
12.2.1. Lexicon: lexique.xml
12.2.2. Rules repository: rules_yyyy-mm-dd.xml
12.2.3. Pre-rules repository: rules_root_yyyy-mm-dd.xml
12.2.4. Rules contextualization: rules_result_yyyy-mm-dd.xml
12.2.5. Rules explanations: rules_explanations_yyyy-mm-dd.xml
12.3. HOW TO IMPLEMENT THE RULES FOR A PROSPECTIVE USE (TRANSACTIONAL USE
OF THE CDSS)?
12.3.1. General considerations
12.3.2. “Cause” conditions of the rule
12.3.3. Outcome of the rule
12.3.4. How to manage several rules that predict the same outcome?
12.4. HOW TO IMPLEMENT THE RULES FOR A RETROSPECTIVE USE (RETROSPECTIVE
USE OF THE CDSS, DASHBOARDS, CONFIDENCE COMPUTATION)?
12.4.1. General considerations
12.4.2. The “event” concept
12.4.3. From data to events
12.4.4. Using events to compute the confidence of a rule
13. APPENDIX 5: VALIDATION OF THE USE OF SEMANTIC MINING FOR ADE DETECTION
13.1. INTRODUCTION
Automated detection of Adverse Drug Events by Data Mining of Electronic Health Records
Emmanuel Chazard, PhD Thesis Page 11 of 262
13.1.1. Objective
13.1.2. Rationale in Semantic Mining evaluation
13.2.MATERIAL AND METHODS
13.2.1. Evaluation, Step 1: extraction of ATC codes from free-text documents: agreement between F-MTI and experts
13.2.2. Evaluation, Step 2- extraction of ATC & ICD10 codes from free text: agreements between F-MTI and EHR
13.2.3. Evaluation, Step 3- validation of the use of the semantic mining results for data-mining-based ADE detection
13.3. RESULTS
13.3.1. Evaluation Step 1- extraction of ATC codes from free-text documents: agreement between F-MTI and experts
13.3.2. Evaluation Step 2- extraction of ATC codes from free text: agreements between F-MTI and EHR
13.3.3. Evaluation Step 3- validation of the use of the Semantic Mining results for data-mining-based ADE detection
13.4. DISCUSSION
13.4.1. Ability of F-MTI to extract codes from free-text reports
13.4.2. Ability of F-MTI to provide ATC codes instead of a CPOE
13.4.3. Ability of F-MTI to be used for ADE detection
13.5. CONCLUSION
14. APPENDIX 6: VALIDATED RULES
14.1. ANEMIA (HB<10G/DL)
14.2. HEPATIC CHOLESTASIS (ALKALIN PHOSPHATASE>240 UI/L OR BILIRUBINS>22 μMOL/L)
14.3. HEPATIC CYTOLYSIS (ALANINE TRANSAMINASE>110 UI/L OR ASPARTATE TRANSAMINASE>110 UI/L)
14.4. HIGH A CPK RATE (CPK>195 UI/L)
14.5. HEMORRHAGE HAZARD (INR>4.9)
14.6. LITHIUM OVERDOSE (TO HIGH A LITHIUM LEVEL)
14.7. HEPARIN OVERDOSE (ACTIVATED PARTIAL THROMBOPLASTIN TIME>1.23)
14.8. HYPEREOSINOPHILIA (ÉOSINOPHILIA>109/L)
14.9. HYPERKALEMIA (K+>5.3)
14.10. HYPOCALCEMIA (CALCEMIA<2.2 MMOL/L)
14.11. HYPOKALEMIA (K+<3.0)
14.12. HYPONATREMIA (NA+<130)
14.13. RENAL FAILURE (CREAT.>135 μMOL/L OR UREA>8.0 MMOL/L)
14.14. VKA UNDERDOSE (INR<1.6)
14.15. NEUTROPENIA (PNN<1500/MM3)
14.16. INCREASE OF PANCREATIC ENZYMES (AMYLASE>90 UI/L OR LIPASE>90 UI/L)
14.17. PANCYTOPENIA
14.18. THROMBOCYTOSIS (COUNT>600,000)
14.19. THROMBOPENIA (COUNT<75,000)
14.20. DIARRHEA (PRESCRIPTION OF AN ANTI-DIARRHEAL)
14.21. DIARRHEA (PRESCRIPTION OF AN ANTIPROPULSIVE)
14.22. BACTERIAL INFECTION (DETECTED BY THE PRESCRIPTION OF ANTIBIOTIC)
14.23. PARACETAMOL OVERDOSE (DETECTED BY THE PRESCRIPTION OF ACETYLCYSTEIN)
14.24. FUNGAL INFECTION (DETECTED BY THE PRESCRIPTION OF LOCAL ANTIFUNGAL)
14.25. FUNGAL INFECTION (DETECTED BY THE PRESCRIPTION OF A SYSTEMIC
ANTIFUNGAL)
14.26. HEMORRHAGE (DETECTED BY THE PRESCRIPTION OF HEMOSTATIC)
14.27. VKA OVERDOSE (DETECTED BY THE PRESCRIPTION OF VITAMIN K)
15. TABLE OF FIGURES