Get Complete Project Material File(s) Now! »
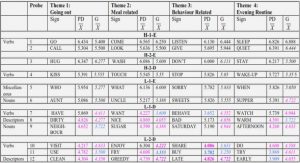
Heterogeneity and subtypes
PD is a very heterogeneous disease, with strong differences in the clinical phenotype, response to treatments and prognosis. For instance, while the average duration of PD from the beginning of motor impairment to death is of 17 years, this period can be shortened to around 7 years in some of the patients. Similarly, while many patients suffer from cognitive impairment from early stages of the disease, others will be relatively unaffected until much later41. To tackle this issue, efforts have been made to split patients into subtypes, based on symptoms that tend to cluster together. Patient stratification is one of the main current frontiers of PD clinical research, the hope being that it will allow to identify specific biomarkers and devise personalised therapeutic approaches41.
The most longstanding classification has been on the basis of the prevalence of tremor in the behavioural phenotype, delineating “tremor dominant” from “non tremor dominant” and intermediate groups41. “Tremor dominant” patients are characterised by slower progression of the disease, relative absence of other types of symptoms and lower functional disability. By contrast, “non tremor dominant”, also known as “akinetic rigid” or “postural instability gait disorder” (PIGD) patients display a globally more severe phenotype, and a higher prevalence of apathy, cognitive decline and dementia13,42.
It has however been argued that the proposed subtypes could simply reflect different stages of the disorder13. For this reason, recent studies have focused on the classification of patients in earlier stages of the disease, using insight from data driven approaches. For instance, a clustering study of de novo PD patients using information based on motor and non motor symptoms identified four subtypes of patients depending on the relative prevalence of motor vs non motor symptoms43 (Figure 2). Interestingly, one of the subgroups was very similar to PIGD patients (“Motor dominant”, MD), characterised by faster disease progression and worse impairment of psychiatric symptoms. Other subtypes were affected by a stronger involvement of non psychiatric NMS, suggesting different biological underpinnings. Furthermore, clustering efforts based solely on NMS support this classification. A recent review of such studies summarised their findings into at least 6 different NMS subtypes of PD, amongst which: cognitive, apathetic, depression/anxiety, REM sleep disorder, pain and weight subtypes44. The three first subtypes, relating to psychiatric components, were all associated with stronger motor and gait impairment, characteristic of the PIGD/MD subtypes45.
Genetic and environmental factors
Population studies have allowed to quantify the relative influence of genetics factors (heritability) on the PD phenotype. For instance, a recent study analysing the family history information of over 1.5 million individuals49 found a PD heritability value of 0.26, leaving a majority of the variance up to environmental interactions or stochastic processes.
Indeed, only a minority (up to 10%) of PD patients have a familial form of the disease, i.e. with an identifiable genetic cause50. Mutations in the SNCA gene, coding for alpha synuclein, were the first to be linked to PD12. It was later found that mutations in the GBA gene, which encodes ß glucocerebrosidase, were associated with the greatest odds ratio (over 5) in PD patients12. Dominant (including SNCA, LRRK2) and recessive (including Parkin, PINK1) mutations have also been associated with inherited forms of the disease. So far, 15 genes have been causally linked to PD50.
Nevertheless, these monogenic forms of PD only account for a minority of patients. Genome wide association studies have allowed to identify additional genetic factors. For instance, a recent meta analysis of GWAS studies of PD found 24 loci that were significantly associated with the disease, including genes mentioned above (GBA, LRRK2, SNCA)12. The presence of multiple risk loci in patients, referred to as the “polygenic load”, has been shown to influence the age of disease onset, but not the rate of disease progression51. A study of genome wide SNPs from over 7000 patients52 yielded a PD heritability value of 0.27, similarly to the study of family histories mentioned earlier. However, currently loci that have been associated with PD only account for a minor fraction of this heritability (3 5%)53, indicating that there still is a significant part of “missing heritability” to uncover, notably in the non coding genome54.
Interestingly, several genetic factors have been linked to symptoms that are more prevalent in subtypes of PD. Indeed, GBA, SNCA and LRRK2 variants have all been linked to worse cognitive impairment and an increased risk of dementia, as well as to other motor characteristics that are more prevalent in PIGD subtypes55.
Staging scenario of Parkinson’s disease progression
This α syn propagation has been suggested to follow a typical pattern over the course of PD. The popular 6 stage scenario proposed by Braak and colleagues in 200359 still holds a major influence on how PD is viewed (Figure 6). According to this scenario, the synucleinopathy would start in the peripheral nervous system, then gradually affect the central nervous system through brainstem nuclei. In particular, Braak hypothesised that PD may start in the gastrointestinal tract. While some research may provide support to this hypothesis, it is still considered controversial and in need of further investigation63.
This pattern particularly fits the symptomatology of PD, especially regarding the time–course of symptom onset. According to this model, in stages 1 and 2, the synucleinopathy would first affect the medulla oblongata, followed by higher brainstem areas including the raphe, reticular and coeruleus nuclei. These initial stages could for instance explain the high prevalence of non–motor dysfunctions in premotor PD17. In the following instances, the nigrostriatal system would be affected (stage 3), leading to the landmark motor and psychiatric features of PD. Finally, in advanced stages (4–6), the wide–spread cortical αα–syn propagation provides a mechanism to explain the progressive development of dementia in patients12.
This staging scenario should however be interpreted with caution. Indeed, only half of PD patients have a synucleinopathy pattern that aligns with the Braak staging model64. Furthermore, the spreading of αα–syn seems to be crucially linked to the vulnerability of specific populations of neurons. For instance, while the striatum is the main projection of substantia nigra neurons, striatal MSN do not seem to be affected by the αα–syn aggregation64. Thus, although the prion–like propagation hypothesis may provide a valid basis to explain the wide–spread distribution of αα–syn aggregates, only neurons with specific features may go on to develop synucleinopathy. Proposed features for such neuronal vulnerability include 3 traits, that are found in substantia nigra DA neurons: complex arborisation of neurons with many vesicular release sites (enriched in αα–syn), high intracellular calcium concentrations due to autonomous pacemaker activity, and high levels of basal mitochondrial oxidative stress64.
Morphology and connectivity
Imaging studies have also been very useful to visualise numerous changes in brain structure, function and connectivity13. For instance, cortical thinning, as well as shrinkage of the amygdala, hippocampus, nucleus accumbens and caudate nucleus head have all been reported in PD99 102. Atrophy of cortical areas and of the nucleus accumbens have even been observed in newly diagnosed PD patients with mild cognitive impairment102. Furthermore, while cerebral blood flow was found to increase in pallidal and putaminal areas, decreases were observed in cortical areas, amongst which the dorsolateral prefrontal cortices67.
Of particular interest to this thesis, resting state fMRI investigations have shown some level of re organisation of cortico striatal networks in PD. For instance, studies have found that while functional connectivity decreased in cortico striatal sensorimotor networks, increases were observed in cortico striatal associative networks103 104. This effect seemed to be related to the extent of DA loss103, and may thus reflect temporary compensatory mechanisms, as other studies have also reported decreases in the functional connectivity of associative circuits106.
Biological bases of PD subtypes
Differences in the patterns of neurodegeneration have been observed in PD subtypes. Indeed, de novo PIGD subtypes exhibit significantly lower dopamine transporter binding in the putamen, but not the caudate nucleus, compared to tremor dominant patients107,108. This pattern of decreased putaminal binding was also replicated in a study looking at the evolution of PD subtypes over a period of 2.5 years109. Post mortem studies have also found differences in the patterns of DA neuron loss in the substantia nigra pars compacta, with PIGD patients having more severe loss in the ventrolateral part, whereas tremor dominant patients showed increased loss in the medial part48.
A recent large scale SPECT study involving 345 early PD patients found that while PIGD patients were characterised by more severe striatal dopaminergic deficits, tremor dominant patients showed stronger loss of serotonin transporter binding. Furthermore, they found that serotonin binding negatively correlated with tremor severity, but not with psychiatric symptoms84. In support of this finding, another study of early PD found that loss of DAT binding in the striatum correlated with hypokinesia and rigidity, but not with tremor108.
Associations with the psychiatric symptoms
Strikingly, all of the PD psychiatric symptoms mentioned earlier have been linked to dysfunctional dopaminergic transmission in the striatum, especially involving the caudate nucleus (CN)115. This is not surprising, as the CN is implicated in executive cognitive processes and goal directed behaviours, directly relating to the dysexecutive and apathetic symptoms observed in patients116. Nevertheless, despite this solid DA base, alterations in other neurotransmitter systems have also been associated with several psychiatric symptoms (Figure 8). For instance, regarding depression, while a substantial body of work has associated this symptom with serotonergic alterations81, other imaging studies did not replicate these findings82,84, possibly due to subtype differences. Levels of inflammation may also play a role, as a study found that leukocyte levels of p11, an adaptor protein that is linked to inflammatory responses and to antidepressant treatments, correlated with depression scores in patients117. Finally, according to a small study, depression, anxiety and apathy may also associated with alterations in noradrenalin dysfunction86.
Although cognitive impairment has consistently been associated with DA loss in the CN, it has also been linked to alterations in dopaminergic and cholinergic markers in the cortex92,102,115,118 120, to shrinkage of cortical and subcortical (amygdala, nucleus accumbens) areas, and to decreases in functional connectivity99,106,121. It is also speculated to be associated with noradrenalin dysfunction122.
Table of contents :
Remerciements
Table of contents
List of abbreviations
List of figures
Résumé en français
INTRODUCTION
CHAPTER 1 – PARKINSON’S DISEASE
A. Symptomatology
1. Motor symptoms
2. Psychiatric symptoms
3. Other non-motor symptoms
4. Heterogeneity and subtypes
B. Biological bases
1. Genetic and environmental factors
2. Cellular pathology
3. Progression mechanisms
4. Brain-wide effects
5. Associations with the psychiatric symptoms
6. A focus on the basal ganglia
C. Treatments
CHAPTER 2 – GPR88
A. Studies of Gpr88
1. Characteristics
2. Insights into Gpr88 function
3. Gpr88 as a therapeutic target
B. Relevance to Parkinson’s disease
CHAPTER 3 – THE RESEARCH PROJECT
A. Objectives
B. Modeling Parkinson’s disease in rats
1. The 6-OHDA toxin
2. Modeling the motor symptoms
3. Modeling the psychiatric symptoms
C. Lentiviral-mediated Gpr88 knockdown
1. The basis: engineered RNA interference
2. The delivery: lentiviral vectors
4 RESULTS
ARTICLE 1 Manuscript : Knock-down of GPR88 alters the response of medium spiny neurons to loss of DA input and L-DOPA.
ARTICLE 2 Manuscript : Gpr88 knock-down in the associative striatum reduces the psychiatric symptoms in a model of Parkinson’s Disease.
GENERAL DISCUSSION
A. Validating Gpr88 as a therapeutic target for Parkinson’s disease
1. Main findings
2. Limitations and future directions
B. Striatal dynamics in basal ganglia disorders
1. Striatal imbalances
2. Biological bases of striatal shifts
3. Therapeutic targeting of the DMS/DLS imbalance
General conclusion
REFERENCES