Get Complete Project Material File(s) Now! »
Chlamydia trachomatis, a human-adapted obligate intracellular pathogen.
trachomatis phylogeny and associated pathologies.
The Chlamydiae: a phylum of its own.
Chlamydia trachomatis is a bacterium belonging to the phylum “Chlamydiae”. This phylum of Gram-negative bacteria branched out very early in evolution, several hundreds of millions of years ago, and one key feature of its members is that they are all obligate intracellular organisms, unable to multiply outside a host cell (Horn and Wagner, 2004). The second characteristic feature of all Chlamydiae is that these bacteria undergo a very peculiar biphasic developmental cycle that is discussed in the next part (Horn, 2008).
This phylogenetic representation of the Chlamydiae phylum is based on the complete 16S rRNA sequence, using Rickettsia sp. as outgroup. Ca. stands for Candidatus, species discovered at the time of the publication and proposed as new species. From Fehr et al, 2013.
The Chlamydiae phylum counts only one Class (Chlamydiia) and one order, the Chlamydiales. Increasing numbers of families are being described thanks to deep sequencing techniques applied to various environmental samples such as sediments, soils or aquatic environments (figure 1) (Bavoil et al, 2013; Horn, 2008; Salamin et al, 2015).
The Chlamydiaceae, a family adapted to animal hosts.
The species belonging to the family Chlamydiaceae have a very condensed genome for bacteria (around 1Mb). In contrast to members of other chlamydial families that can develop in unicellular organisms, Chlamydiaceae only infect animals. Co-evolution with these hosts has led to a massive reduction in the size of their genome (in comparison, the genome of Protochlamydia amoebophila makes 2.4 Mb), and to an increased dependency on metabolic functions of their host (Brian et al, 2004; Stephens, 1998; Omsland et al, 2014).
Infections by Chlamydiaceae lead to the development of diverse pathologies depending on the host and the organs infected. The history of the Chlamydiae started with the discovery of organisms developing in the conjunctival epithelial cells of humans that were later ascribed to the genus Chlamydia. It is only during the 1960s that they were classified as bacteria and not viruses or protozoa given their small size and their unique developmental cycle. All Chlamydia species infect animals including mammals. The range of animals possibly infected varies with the species, and most of the available information deals with species that have an impact on human health or on domesticated animals (Nunes and Gomes, 2014). Five out of the nine Chlamydia species are able to infect humans. C. trachomatis and C. pneumoniae are the two most important species considering the number of cases of infection and the associated symptoms. C. abortus, C. psittaci, and to a lesser extent C. felis, are also able to infect man through zoonotic transmission from infected domesticated or wild animals. For the remaining species, no zoonotic transmission has been reported yet (Everett and Bush, 2001; Nunes and Gomes, 2014).
C. pneumoniae develops in the respiratory tract. Often asymptomatic, it can cause acute respiratory infections in humans and its prevalence in the population is high. It has also been associated to chronic diseases such as atherosclerosis or obstructive pulmonary disease (Choroszy-Król, 2014). It has a large spectrum of hosts: marsupials, frogs, horses, etc (Nunes and Gomes, 2014). C. trachomatis on the other hand only infects humans and is the Chlamydia species with the strongest impact on human health.
trachomatis: a species strictly adapted to humans.
C. trachomatis is the first species of the Chlamydiae that has been discovered in the beginning of the 20th century from conjunctival epithelial cells of patients suffering from trachoma. Given the shape and the Giemsa coloration of the vacuole-containing bacteria and the bacteria within cells, researchers at that time thought they had found a new protozoan surrounded by a cloak, hence its original name of “Chlamydozoa”, coming from the ancient Greek “χλαµυσ” meaning cloak.
This species is the causative agent of different pathologies, depending on the site of infection. Due to a diversity in the immunoreactivity of the major outer membrane protein (MOMP), 15 serovars have been identified so far from clinical samples, and those serovars have been grouped into three different biovars associated with pathologies (figure 2) (Nunes et al, 2008).
The tree was made by comparing 819 genes conserved from the sequenced genomes of different serovars of C. trachomatis, showing a genetic correlation between tissue tropism and infection symptoms, and serovar. From Nunes and Gomes, 2014.
Serovars A to C and ocular infections.
Serovars A, B, Ba and C have a tropism for the eye conjunctiva. These serovars are mainly endemic in developing countries, where they transmit from contact between infected people or through flies that have contacted infected fluids. They are the causative agents of trachoma, an eye disease leading to blindness in long term and non-treated infections. The infection causes an inflammation of the eye conjunctiva and the eyelid, resulting progressively in an entropion, where the eyelid folds inward, and the scratching of the cornea by the eyelashes. This phenomenon called trichiasis means the beginning of an opacification of the cornea leading to blindness if left untreated (Mohammadpour et al, 2016).
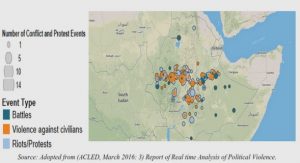
Trachoma is the leading cause of acquired blindness worldwide with 1.8 million people affected and endemic in 51 countries according to the Worldwide Health Organization (WHO). In 2015, 85 million people were diagnosed with an ocular infection by C. trachomatis (Taylor et al, 2014).
Serovars D to K and uro-genital infections.
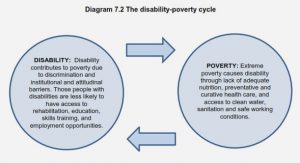
C. trachomatis is also the leading cause of sexually transmitted infections (STIs) of bacterial origin worldwide, with an estimation of 130.9 million new infections in 2012 (figure 3) (Newman et al, 2012).
The estimates are made per region and expressed in millions of new cases per year, data from 2012.
The urogenital tract colonization by C. trachomatis is quite common for both men and women and often asymptomatic – for one man out of two and three women out of four. The infection can remain in the lower parts of the genital tract causing cervicitis in woman and urethritis in men. It can also ascend and generate inflammation of the fallopian tubes (salpingitis), the inner lining of the uterus (endometritis) or the epididymis in men. Tissue scaring, especially in long-term or recurring infections in women, can lead to serious sequelae such as chronic pelvic pain, ectopic pregnancies or even infertility (Mackern-Oberti et al, 2013; Unemo et al, 2017).
Serovars L1 to L3 and lymphogranuloma venereum.
The serovars L1, L2, L2a and L3 are more invasive and are responsible for a STI called lymphogranuloma venereum or LGV. This disease starts with the infection of the genital or colonic epithelium and spreads rapidly towards the blood circulation, disseminating to the draining lymph node by infected circulating monocytes. Once the lymph nodes become infected (10 to 30 days after the initial contamination), the pathology evolves quickly with different symptoms like lymph node necrosis, abscesses or buboes formation, and results in permanent tissue damages (Ceovic and Gulin, 2015; Mabey and Peeling, 2002; Unemo et al, 2017).
Treatments.
Currently, C. trachomatis infections are treated efficiently with antibiotics of the macrolide family such as azithromycin for non LGV serovars, or of the tetracycline family such as doxycycline. No resistance has been reported yet, very likely due to the particular lifestyle of the bacterium, isolated in its intracellular niche (the inclusion, see below). However, the development of a vaccine remains a priority, because many asymptomatic infections are left untreated until the damages are irreversible. Also, infections treated with antibiotics can be followed with reinfections and no efficient immune memory and immunity seems to develop (Unemo et al, 2017; WHO strategy, 2016).
Regarding ocular infections, the WHO has launched a program called SAFE (Surgery – for trichiasis, Antibiotics, Facial cleanliness and Environmental improvement) to eradicate the blinding disease in developing countries in 1996. In 1998 based on the SAFE strategy, a resolution passed for the Global Elimination of Trachoma by 2020 (GET2020). This strategy aimed particularly at increasing the health conditions in the developing countries suffering from trachoma. The WHO report in 2014 pointed out that the situation reported in the 30 countries that participated actively in the survey has improved significantly but major work is still to be done, especially on the F and E components of the SAFE strategy (WHO report, 2014).
Animal models of infection.
Since C. trachomatis only infects humans, the in vivo research on this bacterium has suffered from the lack of suitable animal model. C. muridarum is a species adapted to mice and is genetically very close to C. trachomatis. It has thus been extensively used as an animal model of Chlamydia infection, although important immunological differences between the human and mouse physiology in the reproductive tract exist, and in particular in the innate immune response (De Clercq et al, 2013; Haldar et al, 2016). It is possible to infect mice with C. trachomatis but a higher dose of bacteria is needed and the bacteria are cleared in less than 2 weeks, even in nude mice, implying that the murine innate immune system is sufficient to eliminate C. trachomatis (Tuffrey et al, 1982).
Guinea pig infection with C. caviae was one of the first animal model implemented, and the immune response seems closer to the one happening in human (Miyairi et al, 2010; Shaw et al, 2017). But the paucity of tools in guinea pigs compared to mice, and its higher cost have limited the use of this alternative animal model.
Finally, nonhuman primate models have also been tested. The pig-tailed macaque is arguably the closest to human in terms of physiology (menstrual cycle of 28 to 30 days, anatomy similar) and physiopathology (no need for pre-treating the animals with hormones for example to be susceptible to C. trachomatis genital infections) and is more convenient for breeding (Bell et al, 2011). However, it is scarcely used, due to the practical disadvantages and ethical concerns inherent to macaque studies.
Finally, the last few years have seen the emergence of a new concept, supported by many epidemiological observations, clinical samples and experiments in mice: the possibility that at least some Chlamydia species are commensal bacteria colonizing our gastrointestinal tract. Data from mice experiment using C. muridarum support this hypothesis by revealing a possible gastrointestinal tract long-lasting colonization from a genital tract initial infection (Bavoil et al, 2017; Wang et al, 2018; Zhong, 2017). There is currently no data supporting a gastrointestinal tract colonization by C. trachomatis in humans, but such a scenario would explain among others the reinfection of certain women without any sexual relation after treatment and may account for a large number of chronic infections causing long-term sequelae. This is thus certainly an interesting hypothesis to follow on.
A bacterium with a peculiar biphasic developmental cycle.
Overview of the developmental cycle.
C. trachomatis, along with the other Chlamydiae, undergo an intracellular developmental cycle characterized by the alternation of two different developmental forms, a small (around 0.3 µm of diameter) and infectious form called elementary body (EB) and a dividing form (around 1 µm of diameter) called reticulate body (RB).
After adhesion at the cell surface, the EB gets quickly internalized in a vacuole called “inclusion” (1). The inclusion migrates towards the microtubule organizing center. The EB differentiates into an RB (2), that is the only replicative form of the bacteria (3). After about 24 h, some RBs differentiate back into EBs in an asynchronous manner (4) and ultimately the bacteria, mainly EBs, exit the cell either by lysis (5A) or extrusion (5B). Figure kindly provided by Dr. Mathilde Cossé.
The cycle starts with the attachment of an EB at the surface of a cell, followed by its internalization (figure 4). Once inside the cellular cytoplasm, the bacterium remains in a membrane-bound compartment called inclusion all along the cycle. Within a few hours following entry, the EB gradually differentiates into an RB. The RB divides inside the growing inclusion until, asynchronously, some RBs differentiate back into EBs starting 24 h post-infection (hpi) and until the end of the cycle about 48 h after entry of the bacterium. An intermediate form called intermediate body (IB) corresponding to a transition from RB to EB has been described based on electron microscopy pictures (Kajima et al, 1964). At the end of the developmental cycle, the bacteria, mostly EBs, are released from the cell either by lysis of the cell after breakage of the inclusion membrane and the plasma membrane, or by a so-called extrusion with the release of bacteria still wrapped into an inclusion surrounded itself by another membrane.
Adhesion and invasion of the host cell.
Although C. trachomatis is able to infect mostly epithelial cells in vivo, many different cell types can be infected in vitro, even cells of non-human origin such as mouse embryonic fibroblasts (MEFs). This ability in vitro indicates a diversity of receptors involved in the bacterial adhesion and entry (Guseva et al, 2007). Indeed, several surface proteins have been implicated as potential bacterial receptors as detailed below. The adhesion process proceeds in two steps, a first step which is a loose adhesion based on electrostatic interactions, followed by a firm and irreversible adhesion preceding the invasion step (Dautry-Varsat et al, 2004).
The heparan sulfate (HS) present on the proteoglycan secreted by the cells and on their surface have been shown to play an important role in the adhesion: bacteria no longer attached to cells treated with an HS lyase (Zhang and Stephens, 1992). Other cellular receptors have been identified such as the protein disulfide isomerase (PDI), the platelet-derived growth factor receptor beta (PDGFRb) or the EphrinA2 receptor, using naturally KO cell lines or siRNA screening (Abromaitis and Stephens, 2009; Elwell et al, 2008; Hegemann and Moelleken, 2012; Subbarayal et al, 2015).
On the bacterial side, it has been shown that MOMP exposed at the surface of the EBs was able to interact with HS present on cellular glycosaminoglycans, and cells incubated with recombinant MOMP were resistant to infection by C. trachomatis LGV-L2 (Su et al, 1996; Stephens et al, 2001). Other bacterial determinants have been shown to be important such as the outer membrane complex B (OmcB) and polymorphic membrane proteins (Pmps) (Becker and Hegemann 2014; Fadel and Eley, 2008).
It is important to point out that the requirements in one or another receptor at the cell surface vary in importance depending on the serovars used and may account for the difference in tropism in vivo (Carabeo and Hackstadt, 2001; Fadel and Eley, 2008). Moreover, the diversity of proteins identified on both sides of the interaction reflects probably, at the evolution scale, the absolute requirement for the bacterium to enter a cell in order to complete its developmental cycle.
During this firm adhesion step, the bacterial type 3 secretion systems (T3SSs) present in the EBs, preformed and polarized, get in contact with the cellular plasma membrane, allowing the injection of bacterial effectors such as CT694 or the translocated actin recruiting phosphoprotein (TarP) (figure 5) (Clifton et al, 2004; Fields et al, 2003; Hower et al, 2009; Nans et al, 2014).
Cooperation between host cell proteins and bacterial effectors allow the entry of the bacteria into the cell mediated by a local actin remodeling (Cossé et al, 2016). TarP is able to interact with actin monomers and nucleate the polymerization of filaments (Clifton et al, 2004; Jewett et al, 2006). CT694 interacts with AHNAK, a host cell protein involved in the formation of actin stress fibers and inhibits its F-actin bundling activity. However, the analysis of CT694 KO strains recently suggested that the role of CT694 in entry was not mediated by its interaction with AHNAK (Hower et al, 2009; McKuen et al, 2017). On the cellular side, it has been shown that the small GTPase Rac was activated locally, leading to a recruitment and activation of Arp2/3 complexes through a signaling cascade, also contributing to a local actin remodeling (Carabeo et al, 2004; Carabeo et al, 2007; Elwell et al, 2008). This modification in the actin cytoskeleton allows for the formation of membrane projections that surrounds the bacterium, leading eventually to its internalization in a membrane bound compartment: the inclusion (Carabeo et al, 2002; Nans et al, 2014). More recently, syntaxin-9 (SNX9), a cellular protein involved in filipodia formation and micropinocytosis, joined the growing list of proteins involved in actin remodeling to allow bacterial entry (Ford et al, 2018).
Table of contents :
I. Chlamydia trachomatis, a human-adapted obligate intracellular pathogen
A. C. trachomatis phylogeny and associated pathologies
B. A bacterium with a peculiar biphasic developmental cycle
C. Host-bacterium interactions.
II. Glucose metabolism during Chlamydia infection
A. Glucose in mammalian cells, an energy source and a biosynthesis precursor
B. C. trachomatis and glucose: a long story
C. Glucose metabolism modifications in Chlamydia-infected cell
III. The Tissue Transglutaminase, a cellular enzyme.
A. TG2, a member of the transglutaminase family
B. Regulation of TG2 transglutaminase activity.
C. Physiopathological importance of TG2.
IV. Questions addressed in this doctoral work
I. TG2 is expressed at high level and activated during C. trachomatis infection.
II. TG2 activity sustains bacterial growth.
A. In cellulo.
B. In vivo.
III. TG2 plays a central role in metabolic rewiring during infection.
IV. Glucosamine-fructose-6-P amidotransferase is a substrate of TG2 transglutaminase activity.
V. Modification of GFPT by TG2 enhances the hexosamine biosynthesis pathway.
VI. TG2 activity controls the hexosamine biosynthetic pathway to provide the bacteria with UDP GlcNAc.
I. C. trachomatis infection causes an increase in TG2 level and activity that benefits bacterial growth.
II. TG2 is required to meet glucose demand during infection.
III. TG2 exacerbates C. muridarum pathogenesis.
IV. GFPT1, a substrate of TG2 activity.
V. UDP-GlcNAc production is rapidly consumed in C. trachomatis infected cells.
Concluding remarks
BIBLIOGRAPHY