Get Complete Project Material File(s) Now! »
Patient’s demand and quality standards of health care
A major challenge of health care contracting consists in giving the proper incentives to hospitals to contain costs without sacrificing their quality. For the health authority payer, the problem consists in decentralizing two types of, possibly antagonists, efforts and both difficult to verify and enforce by contract. More precisely, the sequel will consider that the monitoring of standards is too expensive, and even impossible for some aspects of services. This section will discuss the potential virtues of prospective payment in promoting hospitals’ competition to maintain standards of services and therefore alleviate this trade-off.
To be consistent with the restriction of our presentation to the health-care regulation problem with fully insured patients, we will consider hospital competition under administered prices only, i.e. non-price competition. In this context, the role of competition to maintain quality depends mostly on whether the demand of patients reflects quality, and if so, which dimension of the hospitals’ quality.
Cost-reduction vs. quality trade-off when patients’ demand does not reflect quality
In absence of quality competition, the impact of prospective payments depends on the hospi-tal’s own valuation of quality. In principle, under fully prospective payments, a purely for-profit hospital would systematically skimp on non-verifiable quality. Hospitals might achieve cost containment efficiently, but not engage in quality enhancement efforts that would increase their production costs thereby decrease their margin (or at least not beyond the minimum require-ment to avoid for instance being sued for malpractice, or activity ban). However, it is now well recognized and admitted that health-care providers’ objectives include some extent of both benevolence or altruism components, and self-interest.
Despite a certain degree of altruism, Ellis and McGuire (1986) have emphasized that if the physician agency remains imperfect, i.e. if their own relative weighting of patients’ benefit is less than those of the (principal) social planner, some degree of cost-sharing should be im-plemented. By partially relieving health-care providers of the weight from increasing quality in terms of costs, efficiency can be refined and the gap between the physician and the social planner’s valuations of quality be filled. This can typically be achieved by supplementing the prospective payments to some degree of retrospective cost-based repayment. In practice, we observe the authorities’ lump-sum transfers to complement DRG-based system and share with hospitals the cost of undertaking particular activities (Or., 2014). For instance, in France, the MIGAC (Missions d’Intérêt Général et d’Aide à la Contractualisation) program provides finan-cial support to hospitals for undertaking several public interest missions (the « MIG »), or help hospitals to adapt their offer notably with acquiring new technology (the « AC » component) and can be interpreted in this view.
The former reasoning implicitly assumed a one-to-one relationship between cost and quality, but a multi-tasking agency arises if there is no guaranty that any cost’s increase is the reflection of quality improvement. While stressing the duality of both targets, Chalkley and Malcomson (1998b) show evidence that choosing the degree of cost-sharing must solve a second-best trade-off between the promotion of standards of services and limiting the cost of health care. Jack (2005) furthermore extends this problem by addressing that the degree of benevolence may vary upon hospitals and is also unobserved.
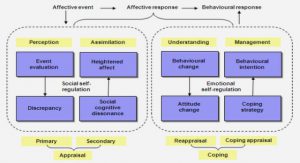
Patients’ demand in health care
There are many reasons to think that the volume of demand to health care practitioners reflects at least some dimensions of quality. However, having a very precise and descriptive model of how patients choose their practitioner or hospital is a complex matter. The parameters involved are numerous and include observable quality, recommendation by general practitioners or relatives, referral and distance to the provider. Moreover, in some health sectors such as hospital-care, patients do not receive frequent treatments so that the quality they observe might not affect their own demand in the future, but instead the demand of other patients. Due to these complexities, most theoretical approaches use reduced forms of demand functions that are increasing in quality in order to capture the relationship between quality and patients’ demand (Ma, 1994, Ma and McGuire, 1997, Chalkley and Malcomson, 1998a, Ellis, 1998). Concerning hospital care, it is admitted that the demand effect should occur through reputation effects or recommendations of the, better informed by experience, general practitioners. Our approach of patients’ response to hospitals’ decisions will follow the same underlying interpretation in the first two chapters of this dissertation.
The use of reduced-demand form has been first introduced in the view of physicians’ induced demand, i.e. the propensity of physicians to increase the volume of care they provide, possibly without affecting these of the other physicians. This view therefore also raises concerns that if the demand increase is not the result of being more attractive than competitors, it can consist in the delivery of unnecessary care. Allard, Thomas Léger and Rochaix (2009) reconcile the re-sult of many static models with reduced demand forms with a more comprehensive/descriptive model of physicians competition in a dynamic setting. Gravelle and Sivey (2010) approach the demand to hospitals in response to their quality by accounting for the imperfection of patients’ information who actually observe noisy signals about qualities. However, this approach from which results are detailed further, introduces tractability issues for other applications such as ours. We should also mention other modelling of hospital competition oriented toward horizon-tal differentiation (Calem and Rizzo, 1995, Beitia, 2003, Brekke, Nuscheler and Rune Straume, 2006, Brekke, Siciliani and Straume, 2011). These works analyze the hospitals’ case-mix dif-ferentiation or specialization degrees and we will not detail these aspects here.
Benefits of prospective payments for promoting competition
By relying on the hospital’s revenue on their activity, the implementation of DRG-based system has substantially increased profit-related incentives in the whole hospital sector. In par-ticular, increasing their demand by attracting more patients has become their main source of surpluses’ increases. We should note here that these incentives are admitted to affect both for-profit and not-for-profit hospitals and because the surplus can be spent on perks for staff or on improving facilities 3.
To the extent that higher repayments increase the incentive for hospitals to attract patients, Ma (1994) shows that the relationship between the hospital’s demand and quality of services gives a supplementary leverage to the authority when setting the fixed repayments. Competition may therefore play a role, through the patients’ demand for quality, to palliate the hospital’s lack of altruism in a measure that depends on the marginal gain to attract patients i.e. the level of prospective payment. In this view, while by design fixed prospective payments allow to decentralize the productive efficiency, an appropriate choice of their level may induce hospitals to internalize the social benefits of quality and alleviate the issue of multitasking. Chalkley and Malcomson (1998a) extend the problem by considering the multiple dimensions of hospital care quality (medical services, nursing, hotel services…). The authors stress that the fact that the patient perceives every aspect of quality correctly (or similarly to the payer) is critical for assessing the role of competition and maintaining the appropriate standards of services. They also show that if patients lack of information about qualities then more complex contracts should be considered.
Information disclosure on measures of hospitals’ quality has been pointed out as the most natural way to address this issue. For instance, the 2003 NHS reform, that introduced patients’ possibility to choose their hospital in the U.K., has been accompanied by the provision of pub-licly assessable information on the provider’s quality to inform the patients’ choices. Ma and Mak (2015) provide a theoretical analysis about how the way information is disclosed may im-pact the outcome and show that a well-designed quality index can also decentralize efficiency under cost-reimbursement. Gravelle and Sivey (2010) analyze a problem with heterogeneous hospitals in duopoly competition and argue that a condition so that a more accurate information effectively promotes quality enhancement is that hospitals’ « endowment » in technology should be similar. The authors explain that, otherwise, better information only reveals the gap between hospitals that, therefore, have less expected gains in improving quality whether it is to confirm their leadership or to try to maintain the confusion for the provider with the lowest structural quality.
The results of empirical studies on the relationship between hospital competition and quality have not led to a consensus. However, the most recent studies tend to find a positive relation-ship (Bloom et al. (2015), Cooper et al. (2011), Gaynor, Propper and Seiler (2012)) with the exception of Gobillon and Milcent (2017) who finds heterogeneous effects depending on the health-care practitioners’ status (distinguishing for-profit, non-for-profit, and public) in France. Those studies generally use indicators of mortality rates of emergency care (generally heart-attack surgery), which have been shown to be a good instrument for hospitals’ standards of quality (Bloom et al., 2011, Cooper et al., 2011)). How to define the relevant hospitals’ market, in particular with regard to the data that are available, remains a difficulty for this literature that we will not examine here. Using different methodologies, the recent studies we mentioned tend to confirm that promoting hospital competition may affect the decisions of patients in the sense of quality enhancement.
The development of new incentive devices
Though competition can be a powerful instrument to maintain standards of quality, it may reveal itself insufficient to induce the efficient levels of all the quality dimensions and has many shortcomings that must be dealt with. On this matter, countries such as the U.S and the U.K have supplemented DGR-pricing systems by value-based-purchasing programs such as pay-for-performance (P4P). They consist in rewarding physicians for meeting certain targets considered as good practices to improve quality indicators. This is the case for instance of the rate of hemoglobin testing for diabetic patients or reduced blood pressure and cholesterol measure-ments in patients with ischemic heart disease (Kaarboe and Siciliani, 2011). However, due to the numerous dimensions of qualities, for which many are not verifiable and thereby not con-tractible, those systems must also deal with the teaching to the test concerns, i.e. the concerns that targeting some verifiable dimensions of quality may only induce hospitals to focus all their effort on these contracted dimensions at the expense of other dimensions. In a model with par-tially altruistic health providers Eggleston (2005)’s finding suggests that altruism may alleviate teaching to the test issues if some degree of cost-sharing is implemented. In an extension of Eggleston’s work, Kaarboe and Siciliani (2011) characterize whether incentive designs, such as P4P, should be implemented for given services in function of the degree of substitutability between the verifiable and non-verifiable dimensions of these services. Glaeser and Shleifer (2001) show that effects of teaching to the test concern both for-profit and non-for-profit hospi-tals, but explain that its main driver may differ between each status. They furthermore explain why health care providers may prefer to choose non-for-profit status since it might have positive connotations for patients and affect their perceptions of quality.
We have briefly reviewed the main issues and conflicts for decentralizing efficient quality standards and costs containment. The potential virtues of competition on this matter have fos-tered its promotion in the actual DRG-based system for funding health care. So far, we have mostly discussed quality dimensions that are unconditional to patients and have a public good flavor, i.e. patients may benefit differently from the quality, but the quality standards are the same for all patients. Vertical differentiation of providers will be considered in the last chapter of this thesis only. One should also observe that the terms of allocative efficiency could also have been used to discuss the objectives of the authority in terms of quality enhancement of care. In this case, allocative efficiency would have referred to the property that the average marginal benefit of quality equals the marginal cost of its production.
In an application to home-care services, the third chapter of this thesis will discuss the decentralization of quality standards to a public-private duopoly, where only the public firm has a ubiquity constraint, i.e. must provide services to the consumers that demand it, whatever the location of the consumers on the territory. We will show that an asymmetry in terms of coverage constraint between public and private competitors can be detrimental to the allocative efficiency in terms of quality standards. In particular, it discourages the quality differentiation between providers that, otherwise, should be efficient given the heterogeneity of consumers’ valuations/marginal benefit from quality.
We have not referred to efficient quality in terms of allocative efficiency so far to avoid any confusion with the dimension of allocative efficiency that we will discuss in the sequel and will be central in the first two chapters of this dissertation. In this view, we will still consider that patients may differently benefit from quality, but now also discuss the allocative efficiency of care by taking into account that the care intensity can differ across patients. The effect of hospital competition in terms of allocative efficiency when evaluated at the level of patient types have been theoretically analyzed first by Ellis (1998) (c.f. infra).
Patients heterogeneity and allocative efficiency of care
This section addresses another fundamental challenge of health-care regulation that is to promote productive efficiency and quality without inducing inefficiency from patients’ selection neither distortions in treatment praxis. We will argue that if concerns of patient selection are inherent to the implementation of DRG-based prospective payments, those from the distortions of treatments’ praxis are the result of their design that is only partially prospective in practice. Allocative efficiency of care questions whether the benefits from public funds spent into a treatment consistently exceed the opportunity cost of other goods or treatment that might be provided. The central criterion is therefore the cost-effectiveness of treatment provision. In practice, the criteria of cost-effectiveness play an increasing role in determining whether patients should receive a treatment or not. In this respect, how to measure and value the patient’s benefits is a constant source of debate and will not be addressed here. The most established measure is the QALYs (Quality-Adjusted Life-Year) (Garber and Sculpher, 2011). In terms of implementation, the National Institute for Health and Care Excellence (NICE) in the U.K. remains the best example of the application of costs-effectiveness criteria. The agency explicitly gives a threshold of between £20000 and £30000 per QALY gain so that a new technology treatment gets funded by the National Health System (Garber and Sculpher, 2011, NICE, 2013). One should, however, notice that the evaluations are conducted on average, and acceptance does not account for heterogeneous gains and costs across patient types as the following discussion will suggest.
Over-provision, under-provision, and excessive rationing will be the main concerns here. The problem of health care regulation they address mostly concerns the asymmetry of informa-tion on patients’ illness and physicians’ discretion over provision, and the problem of decen-tralizing an appropriate use of resources in this context. These concerns will be shared by all chapters of this dissertation. We will first present the different issues related to patient selection in the terms of Ellis (1998), and then present the issues of procedure selection that relies on the classifications designs.
Allocative efficiency at the intensive and extensive margins
The heterogeneity of patients within DGRs is inherent to the principle of PPS that aim at dissociating the repayment to the actual cost of care. We will follow the terminology of Ellis (1998) who proposes to decompose the payments system’s impact on hospital’s use of resources among patients into its intensive margin and extensive margin. The authors describe that due to the heterogeneity of patients within a DRG, hospitals may be led to undertake ‘creaming’, the over-provision of services to low-cost patients, ‘skimping’, the under-provision of services to high cost patients (the intensive margin) and ‘dumping’, the explicit avoidance of high cost patients (extensive margin).
Payments effects at the intensive margin
On the intensive margin effect, Ellis and McGuire (1986), Ellis (1998) and Ma (1994) argue that cost-based retrospective payments may lead to cream all patients. This is due to both the demand-side moral hazard in presence of fully insured patients and to supply-side moral hazard to the extent that physicians also value benefits from treatment that otherwise is incumbent to patients only (altruism) and has discretion over what should be provided. Ellis (1998) moreover suggests that prospective payment systems may lead to skimping on the costlier patients (high severity patients) or dumping. Reducing the treatment intensity of high patient types below its optimal level allows the provider to refine a positive margin but still treat the patient, while dumping occurs if skimping is insufficient to fulfill the physicians’ sustainability constraints. Prospective payment systems here are a fixed price for all patients’ severity types, and can be interpreted as patients belonging to a given DGR.
To avoid any confusion, this dissertation will mainly focus on adverse-selection issues and put hidden actions aside, i.e. we will consider treatments’ intensities that are observable or at least verifiable and contractible. In this view, Choné and Ma (2011) consider a problem of health care contracting when over-utilization, creaming, may arise on observable quantities of care. They analyze the problem of contracting given that both physician intrinsic motivations (or altruism) and the type of illness of the patient are heterogeneous and unobserved. The authors consider that there is a positive relationship between the physicians’ altruism and the average severity of illness of their patients and a possible antagonism between the physicians’ incentive (that are also motivated by their altruism), and liability constraint (that is not). As a result, they find that the optimal contracting issue can lead to some degree of pooling between physicians with different altruism, who should all provide the same quantity of care despite the fact they have different patients case-mix. More precisely, they suggest that maximal quantity of care at the intensive margin can arise at the second best optimum.
Payments effects at the extensive margin
The effects of extensive margin rely on the risk that prospective payments bear on the health providers: excessively costly patients may be associated with significant losses. Therefore, it can induce hospitals to undertake risk selection/dumping i.e. avoiding types of patients for whom the treatment cost exceeds the DRG-price (see for instance Ma (1994), Ellis (1998), Eggleston (2000), De Fraja (2000), Makris and Siciliani (2013)). In addition, to the extent that DRG-prices do not necessarily reflect the average cost of treatments, they may encourage hospitals to specialize into the provision of treatments for which expected costs are lower than DGR prices (Dranove, 1987). In the view of Ellis (1998)’s terminology, one can also interpret specialization as an extensive margin effect.
In practice, dumping mechanisms are not necessarily restricted to strict admission refusals of some patient types. This can actually be contrary to the institutional framework. It can, however, consist in more indirect mechanisms, from the influence of the General Practitioner (GP) referral system, use of waiting lists, choice of the size of the services in terms of beds, or simply closure of loss-making services. Due to its various forms and the difficulty to obtain data on patient selection, there are few empirical assessments of the phenomenon. Newhouse (1989) finds that less profitable patients are more likely to be found in last resort (typically public) hospitals, which suggests a dumping practice of the other hospitals.
The regulation issue lies on the fact that hospitals observe patient types and can anticipate their cost of treatment while the purchaser authority cannot. Chalkley and Malcomson (2002) shows that introducing some degree of cost-sharing could again be a privileged instrument to deal with this issue. The principle is the following: under fully prospective payment, DRG-prices must be high enough to avoid dumping on the most costly patients, but implies to leave hospitals a rent when patients’ treatment costs are low. Some degree of cost-sharing would reduce hospitals’ cost-containment motivations, but limit incentives for dumping when cost is high and allow the authority to pay less when cost is low, thereby also decreasing the rent left. However, such form of cost-sharing is poorly used in health care in practice, mostly because they involve large monitoring costs. In this view, the problem of risk selection has also been addressed by the implementation of outliers payment policies which implement supply-side cost-sharing if the hospital’s loss exceeds a given threshold. Outliers payment policy design raises other issues of implementation, that won’t be detailed in our presentation (see Sappington and Lewis (1999), or Mougeot and Naegelen (2008) for theoretical analyses).
Over-provision of treatment at the extensive margin and rationing in health care
The concerns of patient selection also relates to the question of over-provision at the exten-sive margin. This kind of over-provision addresses the possibility that some degree of patient selection at the extensive margin may actually be efficient. To the extent that the costs of treat-ment may not necessarily exceed its value in terms of patient benefits, or the opportunity cost of providing other goods or treatments to other patients, their coverage could be limited at the optimum and lead to the rationing of treatment provision. Patients would therefore need to pay if they want to access the treatment. Theoretically, rationing can generally be interpreted as the consequence of the costs of some advanced technologies that can be too high relatively to the taxpayer’s willingness to pay (De Fraja, 2000).
Concerning over-provision of treatment at the extensive margin, it is mostly block contracts and cost-volume contracts that are considered and discussed (Chalkley and Malcomson, 1998b). Block contracts consist in fixed prospective payment (lump sum) for the care of all patients within a pathology, independently from their number. Cost-volume contracts generally specify a lump sum and a cap to the number of patients to treat. Given the heterogeneity of patients, a critical theoretical concern for the implementation of block contracts lies into the asymmetry of information between the providers and the regulation authorities about the patient’s character-istics. Given this asymmetry, the first issue to implement cost-volume contracts is to determine what are the patient types that each actor aims at seeing treated in priority. This is a critical aspect that will determine whether hospitals and health authorities are aligned in their sorting of patients and whether volume control can be effective. For the authority, the question is whether the net social benefit from treatment is higher for the more severe or less severe patients. The literature addressing rationing generally considers that, within a pathology, the net social benefit from treatment is decreasing in patient’s severity of illness i.e. the cost increases at a faster rate than benefits (Chalkley and Malcomson, 1998b, De Fraja, 2000, Makris and Siciliani, 2013, Choné and Gauthier, 2017). As a result, the for-profit motivations are aligned with the social planner’s objectives: the hospital would decide to treat first the patients for whom the treatment is the most valuable socially and contracts specifying a number patients to treat can be effec-tive. When altruism is considered it is also necessary that patients with high benefits are also having lower costs, so that the altruistic and profit motives are aligned. When these necessary conditions are met, the use of block contracts may no more be effective. See Mougeot and Naegelen (2014) for an analysis of the problem when these criteria are not met and a study of the non-responsiveness issues that may arise.
Due to specialization or hospital size and economy of scale for instance, some hospitals may be more productive in the provision of certain health services than others. The way payment contracts should account for hospital differences in productivity therefore becomes an additional question. Indeed, the optimal degree of rationing may vary across hospitals, and the most severe cases should be treated in the most productive hospitals only.A key aspect of this matter is that if more productive hospitals must treat a larger number of patients, including costlier patients, they might actually end up with larger total costs which might complicate the use of block contracts with lump-sum payments only. De Fraja (2000) analyzes the problem of optimal rationing when hospitals’ productive efficiency varies and is unobserved while Makris and Siciliani (2013) and Mougeot and Naegelen (2014) extend the analysis to unobserved physicians’ degree of altruism.
In practice, block contracts may also be difficult to implement, as beyond the requirement of responsiveness, it requires that the number of patients to be treated is known in advance. Chalk-ley and Malcomson (1995) therefore argue that their design is better suited to elective/non-emergency care where the capacity for treatments is, in general, limited and fully used. More-over, optimal block contracts depend on the patients’ distribution in each hospital. The distribu-tion of patients’ characteristics/severity of illness may vary across hospitals and can be difficult to observe by the authorities. On the difficulty to assess the proper number of patients to treat in each hospital, Choné and Gauthier (2017) consider a problem where the authority does not know the relevant distribution of patient types. The authors characterize conditions on the dispersion across possible condition so that if the efficient number of patients to treat is large enough, the optimal policy can consist in increasing the number of patients treated.
Another caveat of the use of cost-volume contracts in theory is that their counterpart in praxis generally consists in specifying fixed prices and quantities associated to lump sum transfers (see De Fraja (2000) for a discussion of cost-volume contracts’ implementation). In particular, it generally requires that the authority can set negative lump sum which is not observed in practice. Miraldo, Siciliani and Street (2011) have addressed the problem of rationing where authorities are limited to use fixed prices as their instrument. The authors argue that the analysis is more constrained but more realistic. Following also Malcomson (2005), our approach of rationing in Chapter 1 will be restricted to a fixed price instrument. As the former, we will not discuss the hospitals’ heterogeneity but the heterogeneity of treatment procedures and procedure selection issues that are presented below.
Table of contents :
Introduction – Résumé Substantiel en Français
General Introduction
0.1 Context
0.2 Patient’s demand and quality standards of health care
0.3 Patients heterogeneity and allocative efficiency of care
0.3.1 Allocative efficiency at the intensive and extensive margins
0.3.2 Refinement of DRG classification and health-provider’s procedure selection
0.4 Universal obligation of services and providers status in health care
0.5 Outline of the dissertation
1 Hospital Competition: Treatment Decisions and Coverage of Care
1 Introduction
2 Framework
2.1 Efficient allocation of treatment
2.2 Second best allocation of treatment
3 The impact of hospital competition on welfare
4 Extensions and empirical predictions
4.1 Hospital competition and global coverage
4.2 Different patients’ out-of-pocket participation
4.3 Testable predictions and concluding remarks
2 Incomplete Information and Economic Incentives in Health Care
1 Introduction
2 General framework
2.1 Setting : general structure
2.2 The efficient care procedures
2.3 Informational structure of diagnostic testing
3 Decentralization of care to a monopoly hospital
3.1 Monopoly regulation problem
3.2 Monopoly optimal payment schemes and implementation costs
3.3 Monopoly optimal care procedures
4 Decentralization of care to competitive hospitals
4.1 The competitive regulation problem
4.2 Competitive optimal payments
4.3 Competitive optimal treatment praxis
5 Hospitals’ commitment to cure patients
6 Concluding remarks
3 Mixed Market and Asymmetric Universal Service Obligations
1 Introduction
2 Framework
2.1 Model settings
2.2 Social optimum and limited coverage
2.3 Decentralization to a mixed duopoly
3 Mixed-duopoly equilibrium prices and coverage
3.1 Equilibrium prices and consumers’ segmentation
3.2 Equilibrium coverage
4 Impact of asymmetric USOs on equilibrium qualities
4.1 The firm with USOs provides the high quality qu ≥ qpr
4.2 The firm with USOs provides the low quality qu < qpr
5 Discussion and robustness
6 Concluding remarks
General Conclusion
List of Tables
List of Figures
Abstracts