Get Complete Project Material File(s) Now! »
NF-κB pathway
NF-κB has been considered to play a key role in inflammatory response. TLRs represent an important non-self recognition system that recognizes PAMPs to trigger inflammatory response. After stimulation of LPS, activation of downstream signals to TLR-4 leads to nuclear factor of kappa light polypeptide gene enhancer in B-cells inhibitor, alpha/beta (IκBα/β) degradation and translocation of NF-κB to the nucleus. NF-κB evokes transcription of inducible nitric oxide synthase (iNOS) and pro-inflammatory cytokines (98) (Figure 2). It is demonstrated that activation of the inositol 1,4,5-trisphosphate 3-kinase (IP3K)/ protein kinase B (AKT) pathway is decreased in mesenteric arteries during sepsis probably due to a reduction in translocation (99). However, activation of IP3K/AKT pathway is reported to negatively regulate NF-κB (100, 101). Furthermore, phosphorylation of endothelial nitric oxide synthase (eNOS) is decreased is sepsis, which is reported to be associated with impaired IP3K/AKT pathway (99).
Adaptive immune system
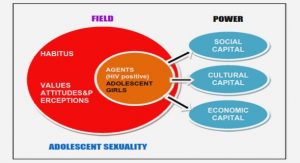
The adaptive immune system is composed of highly specialized lymphocytes and processes. This system is initiated by antigens presented by antigen-presenting cells (APC), such as dendritic cells, monocytes and macrophages. It is also responsible for generating memory T cells and re-calling responses to immediately eliminate re-invading pathogens. The two main groups of lymphocytes are CD4+ T cells and CD8+ T cells. Control cells and helper T cells are two subtypes of CD4+ T cells. Helper T cells are essential for generating specific responses against extracellular (T-helper (Th) 2) and intracellular (Th1) pathogens. CD8+ T cells are known as cytotoxic T lymphocytes, which kill targeted cells, such as tumor cells or virally infected cells. CD8+ T cells are also responsible for antibody production. Antigen-specific antibodies can coat the surface of a pathogen, neutralize toxin and fix complement, which facilitates the phagocyte to phagocytose pathogens. Circulating neutrophils of the innate immune system are typically increased during septic shock. Conversely, the lymphocyte population markedly declines during septic shock. B cells and CD4+ T cells in both pre-clinical models of sepsis and septic patients are significantly decreased (102-104). In 1999, Hotchkiss et al. performed autopsies of patients who died from septic shock and showed that accelerated apoptosis was common in lymphoid organs (the thymus and spleen) and in the lymphoid portions of other organs (the large intestine) (105). Thereafter, in neonatal and pediatric patients who died from sepsis, Pelekanou et al. reported a similar apoptotic pattern (106). In septic shock patients, accelerated apoptosis of circulating lymphocytes is also widespread, resulting in persistent lymphopenia (107). Even though the depletion of lymphocytes is frequently seen in septic shock, the mechanisms are not totally clear (108, 109).
Inflammation paradigm
Traditionally, the hyper-inflammatory phase is considered to be predominant in the initial stage of septic shock (110-112). This phase, called ―cytokine storm‖, is characterized by the production of numerous pro-inflammatory cytokines, such as tumor necrosis factor alpha (TNF-α), IL-6, IL-1β, IL-8, IL-2, and IFN-γ. The extent of the initial pro-inflammatory response is determined by a number of factors, such as the microbial inoculum, pathogen virulence and the patient’s co-morbidities. The intensity of the initial ‗cytokine storm‘ is also associated with a high mortality rate of septic patients (113). During the sepsis process, this pro-inflammatory response is shifted to an immunosuppressive response (114, 115) initially termed ―Compensatory Anti-Inflammatory Response Syndrome‖ (CARS) (111, 116-118).
During the CARS phase, an opportunistic second hit can occur, which is associated with a high mortality rate (119). The paradigm that septic shock is firstly characterized by a hyper- inflammatory stage, and then enters into the second hypo-inflammatory stage is still debated (110, 120) (Figure 3).
Cardiac pathophysiology in septic shock
In 1984, by using radionuclide-gated blood pool scanning and simultaneous thermodilution for cardiac output (CO) measurement, Parker et al. (125) described a myocardial depression in a cohort of 20 septic shock patients. An initial left ventricular ejection dysfunction below 40% was found in 10 of 13 surviving patients. All reversed their cardiac dysfunctions within 7-10 days.
Ognibene et al. also reported that myocardial performance assessed by left ventricular stroke work index (LVSWI) was depressed in septic patients by using right heart catheterization and radionuclide cineangiography (126), a result which was confirmed in 94% of 30 patients by Ellrodt et al. (127),
Jardin et al. observed 90 patients in septic shock by echocardiography and also found a decrease in left ventricular ejection fraction (LVEF) associated with a systematic preload deficiency with a trend toward worsening despite fluid loading in non-survivors (128). Charpentier et al. performed an observational prospective study of 34 patients with septic shock, and found that 44% demonstrated a decrease in fractional area contraction measured by echocardiography (129). In another echocardiographic study of 183 patients, a low cardiac index (CI < 3L.min-1.m-2) and an hypokinetic left ventricular fraction (mean LVEF 38%) were observed in 35% of patients at admission (130). This alteration in myocardial function is only transient and recovers in all surviving patients.
Diastolic dysfunction also occurs in septic shock patients. Pirracchio et al. reported an increase in end-diastolic pressure resulting from a reduction in left ventricular compliance in anaesthetized endotoxemic rabbits (131). The existence of a diastolic dysfunction was also confirmed in human studies. In the study of Jafri et al., abnormal diastolic filling patterns were observed in all patients with septic shock by using pulsed Doppler trans-mitral spectral analysis (132).
Right ventricular dysfunction
Right ventricular performance is also frequently impaired during septic shock. Kimchi et al. reported a series of 25 patients with septic shock in whom 13 developed a right ventricular ejection fraction (RVEF) dysfunction (RVEF <38%) (133). Right ventricular function is particularly influenced by its afterload. Hypoxemia, hypercapnia, left ventricular dysfunction as well as mechanical ventilation with high end expiratory pressure values increase right ventricular afterload, which may worsen left ventricular dysfunction during septic shock.
Thereafter, in a study including 68 septic shock patients, Vincent et al. also observed higher RVEF dysfunction in non-survivors compared to survivors (134). Vieillard-Baron et al. found a right ventricular dilatation in 24% of septic shock patients, even if the difference of RVEF between patients with and without right ventricular dilation was not significant (135). Finally, similarly to the left ventricle, right ventricular dysfunction frequently occurs during septic shock.
Mechanisms of cardiac dysfunction
Septic shock is characterized by vasodilation and depletion of intravascular volume, leading to underfilling the heart with the consequence of a reduction in CO. This induces an imbalance in oxygen demand-supply debt (136), which is usually reversed by fluid resuscitation (5). Nevertheless, it was demonstrated that coronary flow assessed by thermodilution with coronary sinus catheterization was higher or unchanged in patients with sepsis-induced myocardial depression (137). Dhainaut et al. also found a marked coronary vasodilation without elevation of myocardial lactate production in septic patients (138). It seems there is no or little hypoxemia and hypoxia in the septic heart. However, inflammation induces a vascular leakage that may cause myocardial edema resulting in cardiac compliance reduction and dysfunction. Inflammation may also induce dysoxia at cellular and mitochondrial levels (139).
Microcirculation changes
The microcirculation undergoes major changes during sepsis. Groeneveld et al. reported heterogeneous coronary blood flow in endotoxemic dogs, such that flow decreases in some areas but increases in others even at unchanged global blood flow (140). This alteration may be due to intravascular fibrin deposits and endothelial swelling (141). Nevertheless, no cellular hypoxia was found by using marked fluoromisonidazole in septic rats in the Hotchkiss et al. study (142). However, cardiac myocytes interact with vascular endothelial cells. Activation of endothelium results in increased production of endothelin, prostaglandins and nitric oxygen (NO), which act as paracrine regulatory factors of cardiac myocytes (143) leading to cardiac function impairment (144, 145). Vice-versa, activated cardiomyocytes can alter endothelial barrier promoting circulating leukocytes, which migrate into cardiac interstitium through the endothelium. Indeed, increased infiltration of neutrophils (146), monocytes and macrophages (147-149) was found in the myocardial interstitium.
Autonomic dysregulation
Apoptosis of glial cells and neurons in autonomic centers, which regulate the cardiovascular system was reported in septic patients by Sharshar et al., which could result in inadequate autonomic control of the circulatory system (150). Cardiac sympathetic nerve activity has been shown to be highly activated after injection of LPS in animals (9). Elevated circulating catecholamine levels have been documented both in animals (9, 151) and in patients (10, 152, 153). Adrenergic stimulation causes tachycardia, which lowers ventricular filling and increases oxygen requirements. Meanwhile, sustained tachycardia (HR > 95bpm) was reported to be associated with a high mortality rate (154). It was demonstrated that β-AR density was decreased in the heart of septic rats (155) through sequestration and down-regulation. Sequestration refers to the rapid, agonist-induced translocation of β-AR away from the plasma membrane to a distinct vesicular compartment deficient in G stimulation proteins, whereas down-regulation refers to decrease in receptor number due to prolonged agonist stimulation resulting in receptor degradation, probably through a lysosomal pathway (156). It was reported that inhibitory G-proteins (Gi) were increased in both septic animals (157) and non-surviving patients (158), while stimulatory G-proteins (Gs) were reduced in endotoxemic animals (159). These alterations lead to reduced adenylyl cyclase (AC) activity and cyclic adenosine monophosphate (cAMP) levels. In brief, autonomic regulation during sepsis can be altered at different levels of the signaling cascade (Figure 6).
Prostacyclin and cyclooxygenase-2 pathways
PGI2 is produced in arachidonic acid metabolism by COX and prostacyclin synthase (PGIS) in vascular endothelium. PGI2 is transported to the VSMC and functions through a Gs protein-coupled receptor (prostacyclin receptor (IP)). Activation of IP results in a rise in cAMP that leads to relaxation of VSMC.
PGI2 levels were found increased in animals treated with LPS and in patients with septic shock (245). LPS-induced hypotension was attenuated by the selective inhibition of the PGI2 receptor, although neither NOx products nor cytokine levels were affected (246). These results support the idea that the PGI2/IP system contributes to vasoplegia in septic shock. Recent studies have shown that it is the inducible isoform of COX (COX2) that is primarily responsible for the augmented PGI2 production in VSMCs (247). However, LPS-induced hypotension was not attenuated in COX2 knock out (KO) mice (248), Moreover, Ibuprofen, a non-selective prostaglandin synthesis inhibitor, did not decrease mortality in a clinical trial (249).
Reactive oxygen species
It has been reported that inhibition of peroxynitrite formation and genetic suppression of NADPH are able to reverse vascular hyporesponsiveness in an endotoxic and hemorrhagic shock model (250). Suproxide anion can oxidize catecholamines (251), while deactivation of catecholamines by superoxide anion is partly responsible for vascular hyporesponsiveness in an experimental septic shock model (252). This hypovasoreactivity was completely restored by a synthetic selective mimic of superoxide dismutase (SOD), M40403 (252). However, neutralization of superoxide or peroxynitrite has not been assessed in septic patients to date in spite of the promising results in animals.
Sympathetic nervous system
For SNS, the control centers are located in the brain, which are activated by different inputs from sensory afferent nerves (via the hypothalamus), or by central nervous stimuli (cortical areas, limbic system) (253). After activation, the sympathetic control centers stimulate sympathetic efferent fibers, which go through the spinal intermediolateral column and arrive at the sympathetic ganglia. Postganglionic sympathetic nerve fibers enter into organs, such as heart, vessel, lung, liver and kidney. The postganglionic sympathetic fibers release catecholamines, such as Epinephrine and Norepinenephrine, which function via ARs.
β-adrenoreceptors and their signaling pathways
Cardiac sympathetic nerves release catecholamines to regulate cardiac contractility, HR and metabolism via β-ARs. β-ARs consist of four subtypes: β1-AR, β2-AR, β3-AR and the β4-AR (254). The predominant cardiac β-AR is β1-AR, which is found to comprise 75%-80% of β-ARs in heart, followed by β2-AR that occupies 20%-25% of β-ARs in heart. β2-AR is also expressed in lungs, kidneys and blood vessels. β3-AR is found minimally in the heart but primarily in adipose tissue. β4-AR is regarded as a low affinity state of β1-AR, which needs to be further characterized. β-ARs distribution is summarized in Table 5.
Table of contents :
Background
1 Definitions of septic shock
2 Epidemiology of septic shock
2.1 Incidence
2.2 Etiology
2.3 Sites of infection
2.4 Risk factors
2.5 Mortality
3 Immune response in septic shock
3.1 Innate immune system
3.1.1 Activation by microbes
3.1.2 NF-κB pathway
3.2 Adaptive immune system
3.3 Inflammation paradigm
4 Cardiac pathophysiology in septic shock
4.1 Left ventricular dysfunction
4.2 Right ventricular dysfunction
4.3 Mechanisms of cardiac dysfunction
4.3.1 Macrocirculation changes
4.3.2 Microcirculation changes
4.3.3 Autonomic dysregulation
4.3.4 Cytokines
4.3.5 Nitric oxide
4.3.6 Mitochondrial dysfunction
4.3.7 Excitation-contraction coupling impairment
4.3.8 Myofibrillar dysfunction
4.3.9 Cell death
5 Vascular pathophysiology in septic shock
5.1 Vascular regulation
5.2 Vascular hyporeactivity
5.3 Mechanisms of hypovasoreactivity
5.3.1 α1- adrenergic receptor desensitization
5.3.2 Nitric oxide
5.3.3 Prostacyclin and cyclooxygenase -2 pathways
5.3.4 Reactive oxygen species
6 Sympathetic nervous system
6.1 β-adrenoreceptors and their signaling pathways
6.2 Sympathetic system in sepsis
6.3 Interaction between sympathetic system and immune system
6.4 How β-adrenoreceptor pathways interact with inflammation
7 Modulation of the sympathetic system at the β1-adrenoreceptor level in septic shock
7.1 Experimental studies
7.2 Clinical studies
8 Pharmacology of used drugs
8.1 Esmolol
8.2 Ivabradine
Objective of the thesis
Methodology
1 Blood pressure measurement by plethysmography
2 Septic shock model
3 Echocardiography
4 Intra-arterial blood pressure measurements
5 Lactatemia assessments
6 Myograph
7 Enzyme-linked immunosorbent assay
8 Protein extractions and concentration measurements
9 Western blots
10 Total RNA extractions and concentration measurement
11 RT-PCR
Study 1
1 Introduction
2 Methods
2.1 Experimental design
2.2 Ivabradine dosage
2.3 Statistic analysis
3 Results
3.1 Model Characterization
3.2 Hemodynamic effects following Ivabradine therapy in septic shock animals
3.3 Vasoreactivity effects following Ivabradine therapy in septic shock animals.
3.4 Effect of Ivabradine on circulatory inflammatory mediators
3.5 Effect of Ivabradine on CLP-induced inflammatory pathways in cardiovascular tissues
Study 2
1 Introduction
2 Methods
2.1 Experimental design
2.2 Esmolol dosage
2.3 Statistic analysis
3 Results
3.1 Model characterization
3.2 Hemodynamic effects following different doses of Esmolol in septic shock animals.
3.3 Vasoreactivity effects following different doses of Esmolol in septic shock animals
3.4 Effect of different doses of Esmolol on circulatory inflammatory mediators
3.5 Effect of different doses of Esmolol on CLP-induced inflammation in cardiovascular tissues
3.6 Adrenergic modulation following different doses of Esmolol infusion.
Discussion
1 Principle results
2 Model characteristics
3 Isolated heart rate reduction by Ivabradine does not improve cardiac or vascular function
4 Isolated heart rate reduction by Ivabradine does not exert any impact on inflammatory patterns
5 Hemodynamic effects of low doses of Esmolol in septic shock animals
6 Immunomodulatory effects of low doses of Esmolol
7 Heart rate reduction or inflammatory modulation of Esmolol
8 Modulation of adrenergic receptor mRNA expression with Esmolol
9 Study limitations
References