Get Complete Project Material File(s) Now! »
CHAPTER 3 THEORETICAL FRAMEWORK FOR PROVISION OF ESSENTIAL MEDICINES
INTRODUCTION
Research studies have to be based on some form of a framework to guide the study. The framework is defined as an abstract, logical structure of meaning that guides the development of the study and enables the researcher to link the findings to the body of knowledge (Grove et al 2013:41). The framework can be conceptual or theoretical depending on the purpose and design followed. Conceptual Framework is defined as logical grouping of related concepts that is usually created to draw together several different aspects that are relevant to a complex situation whereas the theoretical framework is a knowledge form within the empirical form which is created to draw together several different aspects that are relevant to a complex situation (Chinn & Kramer 2011:246, 257). In this study the situation is the provision of essential medicines.
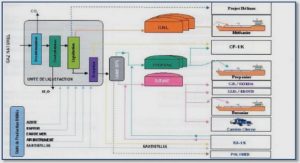
For this study a theoretical framework chosen was the Pharmaceutical Framework as developed and further refined by Management Science for Health in 2012 which comprise of the following aspects: Selection, Procurement, Distribution and Use of the provision of essential medicines guided by the legal framework.
THEORETICAL FRAMEWORK FOR DRUG (MEDICINE) SUPPLY MANAGEMENT
Management Science for Health in 2010 conducted extensive studies on medicine provision and availability across the world and after which the member states and regional consultations adopted a Medicine Supply Management Framework which is based on a four step framework which include activities for the selection, procurement, distribution and use as developed by the Management Sciences for Health.
At the centre of these processes are management systems, finance, human resources management, information management and policy governance functions (MSH 2012:1.8). This framework guides the provision of the medicines across the member countries in a holistic approach through clearly outlined processes for selection, procurement, storage, distribution and usage of medicine. When implemented properly the possibility of ensuring continuous access and provision of medicine is likely to be successful.
There has been further developments within medicine supply management sector towards refinement of the framework to guide medicine supply provisioning the development was facilitated by the MSH as the main organisation internationally lobbying for the medicine provisioning reforms and strongly advocating for the promotion of equitable access to quality medicine as both a key development challenge and an essential component of strengthening the health systems and primary health care reform in the world The framework was finally adopted by World Health Organization in 2011. The purpose of the framework was to standardise processes within member countries for the medicine provisioning systems with an intention to ensure consistent medicine availability at all levels. WHO believed that to preserve lives it is a key principle that the provision and continuous availability of medicines be placed as an important priority that countries should design and implement the National Medicine Policies to guide selection, procurement, distribution and use of medicines. As a core component of the framework, the National Medicine Policy is regarded as an indication for political commitment and a guide for action that can demonstrate how the government will ensure that efficacious and safe medicine of good quality are affordable, accessible, available and rationally used (MSH 2012:1.9).
To this end the majority of WHO member countries including South Africa have approved national medicine policies.
According to MSH (2012:1.10), pharmaceutical management framework comprises four basic functions: selection, procurement, distribution, and use. Selection involves reviewing the prevalent health problems, identifying treatments of choice, choosing individual medicines and dosage forms and deciding which medicines will be available at each level of the health system. Procurement Includes quantifying medicine requirements, selecting procurement methods, managing tenders, establishing contract terms, and ensuring pharmaceutical quality adherence to contract terms. Distribution includes clearing customs, stock control, store management, and delivery to depots, pharmacies, and health facilities. Use includes diagnosing, prescribing, dispensing, and proper consumption by the patient. In the pharmaceutical management cycle, each major function builds on the previous function and leads logically to the next. Selection should be based on actual experience with health needs and medicine use; procurement requirements follow from selection decisions, and so forth.
At the centre of the pharmaceutical management cycle is the core of related management support systems, including the planning and organisation of services, financing and financial management, information management, and human resource management. These management support systems hold the pharmaceutical management framework together.
Although individual parts of the framework may function independently for a short time, the cycle as a whole will soon cease to operate and patient care will suffer without effective leadership, a functional organisational structure, adequate and sustainable financing, reliable management information, and motivated staff. The entire framework rests on a policy and legal components that establishes and supports the public commitment to essential medicine supply. The WHO member states subscribe to the above framework to manage provision of essential medicines .The paragraphs below will discuss each component and reflect key requirements for consistent provision of essential medicines.
Selection component
The framework for medicines has to provide for the selection process of essential medicines. Selection should be based on thorough discussions and acceptance by a multidisciplinary committee of experts who has the ability to interprete data and evaluate safety and eficacy of medicines within their area of expertise. The selection of the medicines depend on many factors including the prevalent diseases, treatment facilities, training and experience of the available personnel, financial resources, population genetic ,demographic and environmental factors. The outcome of selection component is the essential medicines lists (EMLs) which support the systematic delivery of medicines in the health-care system (MSH 2012:16.2).
The selection process of the WHO Model List of Essential Medicines has evolved since 1977 from expert evaluation to evidence-based selection that includes: systematic review of evidence of efficacy and safety; consideration of public health needs, availability and costs; and a transparent process.The Model List and its supporting documents serve as a valuable resource for advocacy, selection, purchasing and supply at the country level. In 2016, according to the World Health Organization report, all 194 countries had a national EML and the majority had been updated in the previous five years (WHO 2016:1). The model list has been expanded to include the WHO Model List of Essential Medicines List for Children (EMLc), to address the priority health-care needs of children (WHO 2016:1).
WHO member countries have developed what is referred to as national lists of essential medicines.The lists are commonly used in public sector procurement across all countries and in high-income countries for public insurance reimbursement. However, only a small fraction of countries use the EML for reimbursement for private insurance. All responding countries reported having a committee for the selection of medicines for the national EML. It is important that the EML is regularly updated to ensure that it is relevant to the health needs of the population, adapted to changes in therapeutic modalities, concordant with local treatment guidelines, and aligned with the logistics and budget of the health system.
The WHO survey showed that 69 percent of responding countries had updated their list within the previous five years. 81 percent of low-income countries had revised the EML within the past five years.The production of a national EML can help countries make the best use of limited resources to procure and make available the most appropriate treatments for the priority diseases and conditions. However, regular revision is essential to ensure that the selection remains current and credible (WHO 2011a:6). The concept of essential medicines provides the parameters as to which medicines should be included in the country list. These should be the medicines to treat the major diseases and conditions that affect the population and those that the health system can afford.
Benefits and impact of the cordinated selection of medicines
MSH (2012:16.4) highlights the benefits and advantages of limited selection of essential medicines can be categorised into the following categories supply, prescribing ,organisational and patiet use.
Supply
Easier procurement, storage and distribution, lower stock levels better quality assurance and easier dispensing.
Prescribing
Training of the prescribers will be more focused and simpler with the limited basket of medicines for use to an extent that professionals will gain more experience with fewer medicines.There will be non availability of irrational treatment alternatives, reduced anti microbial resistance as well as focused medicine education and information and better identification of adverse medicine reaction.
Organisational benefits
The selection and specifying the type and number of pharmaceutical to be purchased will lead to an improved quantification process.There will be lower costs due to more competition to provide the limited medicine lists.
Patient use
The limited essential medicine selection and lists will promote medicine availability and reduction in the treatment confusion and further improve adherence to treatment as patients will have fewer medicines to comphrehend as well as patient education will improve with focused education efforts and limited guidelines.
Procurement component
Effective procurement process is meant to ensure the availability of right medicine in the right quantities at reasonable prices and in compliance with the recognised quality standardsThe procurement process is an integral part of the supply chain and pharmaceutical cycle. Good procurement is dependent on selection of the appropriate medicines. It is also important to ensure that the medicinal needs of the country are based on a strong quantification system.
A reliable supply chain system makes it possible to track the status of deliveries, stock, and consumption.It is important that the data from the users and adherence to standard treatment guidelines (STGs) is utilised as a measure of consumption data to be used for the next round of forecasting and selection (Van der Walt 2014:8).
The process of purchasing supplies utilises National,Multinational,private or public suppliers,global agencies depending on availability and costs.Purchasing through global agencies require that mechanisms are put in place to ensure that the quality assurance and control requirements are met to protect the service users and countries through procurement planning, purchasing inventory control traffic, receiving,incoming inspection and salvage operations (MSH 2012:18.6).
Procurement cycle
The procurement cycle involve the following 10 steps:
Review medicine selections to determine quantities needed
Reconcile needs and funds
Choose procurement method
Locate and select suppliers
Specify procurement/contract terms
Monitor order status
Receive and check medicines
Make payment
Distribute medicines
Collect consumption information
Where the procurement cycle is followed the outcome is likely to be an effective procurement process for medicines which will ensures that:
the right medicines in the right quantities are sourced
the buyer-seller relationship are managed in a transparent and ethical manner
the lowest practical purchase price are sourced
all pharmaceuticals procured meet recognised standards of quality
there are timely delivery to avoid shortages and stock-outs
there is supplier reliability with respect to service and quality
the purchasing schedule, formulas for order quantities of purchasing are set at each level of the system
there is efficiency in the procurement processes
Medicine sourcing – procurement strategies
Sourcing of medicines could be done through open tender,restricted tender, competitive negotiation or direct procurement as explained below:
Open tender
A formal procedure by which quotes are invited from any supplier’s representative on national or international, subject to the terms and conditions specified in the tender invitation.
Restricted tender
In a restricted tender, interested suppliers must be approved in advance, often through a formal prequalification process that considers adherence to good manufacturing practices, past supply performance, financial viability, and related factors.
Competitive negotiation
In competitive negotiation, the buyer approaches a limited number of selected suppliers (typically at least three) for price quotations. Buyers may also bargain with these suppliers to achieve specific price or service arrangements. For example, global organisations such as UNICEF, the Clinton Foundation, and supply chain management systems (SCMS) have successfully negotiated reduced prices of antiretroviral (ARV) medicines with manufacturersctors.
Direct procurement
Involve direct purchase from a single supplier, either at the quoted list price or at an agreed standard discount off the list price. For single-source medicines (generally those under patent with no licensing agreements that allow other firms to manufacture the medicine), the buyer basically has two choices namely direct procurement or selection of an alternative drug product (MSH 2012:18.6).
Distribution component
Distribution is meant to ensure a consistent of medicines and supplies to the facilities where they are needed whilst ensuring that resources are used in the most effective manner. Distribution system or framework has four elements which are system, information, storage and delivery elements (MSH 2012:22.2).
The decision of which distribution system will be utilised has to take into account the geographic coverage ,land type and distance, population coverage in terms of persons numbers as well as level of the health systems.
The distribution system has four major elements:
System type which refer to a geographic and population coverage number of levels within the health system and situation analysis of whether processes are centralised or decentralised.
Information systems. The information systems should be able to capture, generate data to demonstrate inventory or stock control to enable production of consumption reports and as far as possible have linkage between the warehouse systems and that of the health facilities.
Storage systems. The environment under which the medicines are stored whilst awaiting distribution has to ensure that the medicines are protected from breakages,extreme heat or cold temperature and exposure to the external elements.The storage system should take into account selection of appropiate sites for storage, building design and layout for optimum temperature and movement of stock as well as the material handling systems for effective order picking and processing.
Delivery systems. These should be developed taking into account the whether medicines will be collected by facilities or delivered by the warehouse utilising organisational resources or outsourced to the third party as well as the routes and scheduling of deliveries. The decision whether to utilise in house or third party should consider type of vehicle, mode of transport required whether road or air, need for vehicles procurement and maintanance which the health department may not necessarily have a skilled resource to manage.
Distribution system options
There are two options for distribution it can either be a push or pull systems (MSH 2012:22.9).
Push system
Push system is achieved by procuring and distributing standard pre-defined quantities of essential medicines for routine use .In the push system operational units are expected to supply certain stock and consumption information to the supply source so that issuing officers can plan allocations when supplying areas with limited access, limited management information system, and/or diversion and theft. Delivery plan is made at the beginning of a planning period (usually a year) and supplies are delivered according to the plan.
Conditions
Staff members at the lower level of the distribution system are not (yet) competent in inventory control.
Demand greatly exceeds supply, making rationing necessary.
A limited number of products are being handled.
Disaster or epidemic relief is needed, or the situation calls for short-term supply.
Transition from a push system to a pull system is recommended once management capacity and record-keeping improve.
Pull system
Pull system is a system through which facilities placed orders from a central warehouse based on the minimum and maximum ordering quantities at regular intervals.
Preconditions for success of the pull system
To be effective this system requires that field staff members are regularly supervised and performance monitored,good data should be available to decision makers,Staff members at the lower level of the distribution system should be competent in quantifying and forecasting needs and managing inventory, sufficient supplies are available at supply sources to meet all programme needs and there must be capacity to handle large range of products.
Distribution cycle
According to MSH (2012:2.5), distribution cycle is a continous process comprising of the following processes:
Procurement of medicines and commodities to facilitate availability for delivery to the health facilities.
Port clearing include identification of shipments as soon as they arrive in port ,processing of all importation documents, completing any customs requirements,storage of medicines properly until they leave the port, assessment of the shipment for losses or signs of damage and after clearance has been issued medicines can then be collected.
Reception and Inspection the new shipment should be kept separate from other stock until inspection has been completed to check for damaged and missing items further the assessment for compliance with contract conditions regarding medicine type, quantity, presentation, packaging, labeling is also executed.
Inventory control processes facilitate coordination of the flow of pharmaceuticals through the distribution system with key objectives of ensuring protection against theft and corruption and facilitate, requisitioning and issuing of medicines, financial accounting and preparing consumption and stock balance reports.
Storage promotes proper location, construction, organisation, and maintenance of storage facilities in order to maintain medication quality, minimise theft and loss through damage and maintain regular supply to health facilities.
Requisition utilise either a push or pull system through forms and procedures which are key components of the inventory control system and provide audit trail for tracing the flow of medicines.
Delivery options can be warehouse staff or collected by health facility staff depending on the cost effective choice made by the entity.
Dispensing the distribution process achieves its purpose when medicines reach hospital wards, outpatient clinics, health centers, or community health workers and are appropriately prescribed and dispensed to patients.
Consumption reporting is a closing link in the distribution cycle enabling flow of information on consumption and stock balances back through the distribution system to the procurement office for use in quantifying procurement needs.
TABLE OF CONTENTS
CHAPTER 1 ORIENTATION TO THE STUDY
1.1 INTRODUCTION
1.2 BACKGROUND INFORMATION ABOUT THE RESEARCH PROBLEM
1.3 STATEMENT OF THE RESEARCH PROBLEM
1.4 AIM OF THE STUDY
1.5 SIGNIFICANCE OF THE STUDY
1.6 DEFINITION OF KEY CONCEPTS
1.7 THEORETICAL FOUNDATIONS FOR THE STUDY
1.8 THE RESEARCH DESIGN AND METHOD
1.9 SCOPE OF THE STUDY
1.10 STRUCTURE OF THE THESIS
1.11 CONCLUSION
CHAPTER 2 LITERATURE REVIEW
2.1 INTRODUCTION
2.2 PROBLEM OF ACCESS AND PROVISION OF MEDICINES
2.3 INTERNATIONAL WORLD HEALTH ORGANIZATION CONTEXT ON PROVISION OF ESSENTIAL MEDICINES
2.4 WHO REGIONAL CONTEXT FOR PROVISION OF THE ESSENTIAL MEDICINES
2.5 WORLD REGIONS MEDICINE PROVISIONING CONTEXT
2.6 AFRICAN COUNTRIES’ MEDICINE PROVISIONING CONTEXT
2.7 THE REPUBLIC OF SOUTH AFRICA’S NATIONAL CONTEXT OF MEDICINE PROVISIONING
2.8 PROVINCES OF THE REPUBLIC OF SOUTH AFRICA’S SITUATION ON MEDICINE PROVISIONING
2.9 CONCLUSION
CHAPTER 3 THEORETICAL FRAMEWORK FOR PROVISION OF ESSENTIAL MEDICINES
3.1 INTRODUCTION
3.2 THEORETICAL FRAMEWORK FOR DRUG (MEDICINE) SUPPLY MANAGEMENT
3.3 CONCLUSION
CHAPTER 4 RESEARCH METHODOLOGY
4.1 INTRODUCTION
4.2 RESEARCH DESIGN
4.3 RESEARCH APPROACH ACTION RESEARCH
4.4 STUDY POPULATION AND SAMPLING
4.5 DATA COLLECTION
4.6 DATA ANALYSIS
4.7 TRUSTWORTHINESS
4.8 ETHICAL CONSIDERATIONS FOR THE RESEARCHER
4.9 SCIENTIFIC HONESTY OF THE RESEARCHER
4.10 ENSURING RIGOR OF ACTION RESEARCH DATA
4.11 SIGNIFICANCE OF THE STUDY
4.12 SCOPE AND LIMITATIONS
4.13 CONCLUSION
CHAPTER 5 DATA ANALYSIS, PRESENTATION, DESCRIPTION OF THE RESEARCH FINDINGS AND EFFECTS OF THE ACTION AREAS
5.1 INTRODUCTION
5.2 DATA MANAGEMENT AND ANALYSIS
5.3 DESCRIPTIVE STUDY POPULATION DATA
5.3.1 Participants professional profile
5.4 PRESENTATION OF FINDINGS AND ACTION AREAS
5.5 SUMMARY OF ACTION AREAS ARISING FROM THE STUDY
5.6 CONCLUSION OF THE RESEARCH FINDINGS PHASE
5.7 DISCUSSION OF IMPLEMENTED ACTION AREAS AND EFFECTS
5.8 CONCLUSION
CHAPTER 6 PROPOSED FRAMEWORK FOR PROVISION OF ESSENTIAL MEDICINES FOR THE DISTRICT HEALTH SERVICES
6.1 INTRODUCTION
6.2 REPUBLIC OF SOUTH AFRICAN DISTRICT HEALTH SERVICES CONTEXT
6.3 LEGISLATIVE AND POLICY FRAMEWORK
6.4 SCOPE OF THE PROPOSED FRAMEWORK
6.5 FRAMEWORK MISSION
6.6 FRAMEWORK VISION
6.7 UNDERPINNING VALUES
6.8 INTENDED GOALS
6.9 STRUCTURE OF THE POLICY FRAMEWORK ON PROVISION OF ESSENTIAL MEDICINES FOR THE DISTRICT HEALTH SERVICES
6.10 MONITORING AND EVALUATION OF THE FRAMEWORK
6.11 CONCLUSION
CHAPTER 7 CONCLUSION AND RECOMMENDATIONS FROM THE STUDY
7.1 INTRODUCTION
7.2 THE RESEARCH DESIGN AND METHOD
7.3 SUMMARY AND INTERPRETATION OF THE RESEARCH FINDINGS
7.4 STUDY RECOMMENDATIONS
7.5 CONTRIBUTION OF THE STUDY
7.6 LIMITATION OF THE STUDY
7.8 CONCLUDING REMARKS
REFERENCES
GET THE COMPLETE PROJECT